Palliative Care
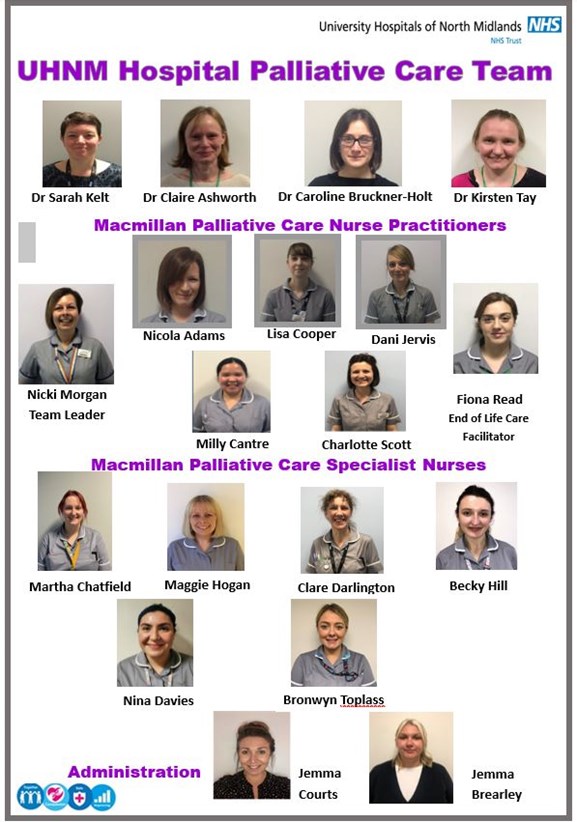
Specialist Palliative Care Team- UHNM
Dr Sarah Kelt- Consultant in Palliative Medicine
Professional Qualifications: MRCP Royal College of Physicians London 2005, CCT and included on the Specialist Register for Palliative Medicine 2009
Academic Qualifications: MBChB University of Dundee 2002
Relevant Additional Training: Level 2 psychological support training, “First aid” cognitive behavioural therapy (St Christopher’s Hospice), Advanced course in pain and symptom management (Sobell House), Foundation course in acupuncture (BMAS), Training consultant teachers, 6th Palliative Care Congress, Quality assurance training for good clinical practice in research, Bristol opioid conference, Advanced communication skills training (Compton Hospice, GMCN), focussed abdominal ultrasonography in palliative care.
Professional Career: After qualifying, Sarah worked as a junior doctor in UHNM working in a variety of specialities including Oncology, Renal Medicine, Neurology, A&E, General Medicine and GI surgery. After completing professional qualifications Sarah started speciality training in Palliative Medicine in the West Midlands. She completed posts at Severn Hospice, New Cross Hospital, Compton Hospice and Douglas Macmillan Hospice. Since becoming a consultant in 2009 Sarah has worked at both the UHNM and Douglas Macmillan Hospice. Sarah is the clinical lead for the Palliative Care Team and for End of Life at UHNM.
Dr Claire Ashworth – Consultant in Palliative Medicine
Professional Qualifications: Membership of the Royal College of Physicians (UK) 1998, CCT and included on the Specialist Register for Palliative Medicine 2004
Academic Qualifications: MBBS University of Newcastle upon Tyne 1995, MSc Palliative Medicine 2003, Postgraduate diploma Medical Education 2023.
Relevant Additional Training: Advanced communication skills, advanced course in pain and symptom management, focussed abdominal ultrasonography in palliative care.
Professional Career: After qualifying, Claire worked as a junior doctor in the Northeast in a variety of specialities including General Medicine, Elderly Medicine, General Practice, and Elderly Psychiatry. After completing professional qualifications Claire spent 6 months working in Hospice Uganda in Kampala before starting speciality training in Palliative Medicine in Oxfordshire. Claire has worked as a Consultant in Palliative Medicine in North Staffordshire since 2005. She was the Medical Director at Douglas Macmillan Hospice from 2006-2018. Currently she works in the UHNM hospital specialist palliative care team and is an honorary senior lecturer at Keele University within the School of Medicine.
Dr Caroline Bruckner-Holt - Consultant in Palliative Medicine
Professional Qualifications: Membership of the Royal College of Physicians UK (MRCP) 2009, MRCP Palliative Medicine 2012, CCT and included on the Specialist Register for Palliative Medicine 2015.
Academic Qualifications: MBBS University of London 2004, BSc Neuroscience University College London 2001, MSc Palliative Medicine University of Bristol 2014
Relevant Additional Training: Advanced communication skills, advanced course in pain and symptom management, focused abdominal ultrasonography in palliative care, clinical hypnosis and stress management
Professional Career: After qualifying, Caroline worked as a junior doctor in the London and the West Midlands in a variety of medical specialities. Palliative Medicine specialty training was undertaken in the West Midlands and Caroline is now Medical Director at Katharine House Hospice, Stafford and at UHNM.
Dr Kirsten Tay - Consultant in Palliative Medicine
Professional Qualifications: Membership of the Royal College of Physicians London 2005, CCT and included on the Specialist Register for Palliative Medicine 2015
Academic Qualifications: Medical State Exam Germany 2001
Relevant Additional Training: Advanced communication skills training, Advanced course in pain and symptom management (Sobell House), Foundation course in acupuncture (BMAS)
Professional Career: After qualifying, Kirsten has worked as a junior doctor in Dorset and Essex in a variety of specialities including Respiratory Medicine, Diabetes & Endocrinology, Elderly Care, Cardiology and Renal Medicine. After completing her MRCP Kirsten moved to Scotland and worked in Oncology and Palliative Medicine for two years before commencing specialty training in the West Midlands. Since becoming a consultant in 2015 Kirsten has worked mostly at Katharine House Hospice and with the Stafford community Palliative Care team.
Nicki Morgan- Macmillan Palliative Care Advanced Nurse Practitioner/ Team Leader
Professional Qualifications: Registered Nurse - Adult, Specialist Practitioner - District Nursing, Principles of Physical Assessment, Nurse Independent / Supplementary Prescriber (V300)
Academic Qualifications: Diploma in Adult Nursing; ENB 998 Teaching and Assessing in Clinical Practice; ENB R01 Clinical Supervision Skills for Supervisors Course; ENB A18 Diploma in Palliative Care; BSC (Hons) Nursing Studies; BSC (Hons) Community Health; MA Ethics of Cancer and Palliative Care (Merit).,
Relevant Additional Training: Level 2 Psychological Support Training; Advanced Communication Skills Training (Compton Hospice / Greater Midlands Cancer Network);‘First Aid’ Cognitive Behavioural Therapy (St Christopher’s Hospice); The Oxford Advanced Courses in Pain and Symptom Management (Sobell Study Centre).
Professional Career: Nicki’s nursing practice is grounded in Gynae - Oncology and community nursing which led to an interest in palliative care. In 1999 as Team Leader, Marie Curie Cancer Care (West Midlands), Nicki developed her knowledge and skills in community palliative care and in 2003 progressed further into specialist palliative care as a PCNS at the Douglas Macmillan Hospice. Nicki joined the team here at the UHNM in June 2012 and in July 2013 was appointed as Lead NP for the palliative care team.
Lisa Cooper- Macmillan Palliative Care Nurse Practitioner
Professional Qualifications: Registered Nurse – Adult; Nurse Independent / Supplementary Prescriber (V300)
Academic Qualifications: BSC (Hons) Nursing Studies; Currently undertaking MSc Palliative and End of Life Care - has successfully completed Palliative and End of Life Care and Symptom Management Modules; Physical Assessment. Teaching and Assessment in Clinical Practice (ENB 998) Lisa is currently undertaking her Masters in Palliative Care – due to complete in 2025
Relevant Additional Training: Level 2 Psychological Support Training; Advanced Communication Skills Training.
Professional Career: Lisa has worked within specialist palliative care at the UHNM for the last 14 years. She qualified in 2004 and her back ground is vascular surgery, district nursing and working with the community matron team focusing on nursing home residents. Her specialist interest is in end of life care particularly within the elderly and NIV patients.
Nicola Adams - Macmillan Palliative Care Nurse Practitioner
Professional Qualifications: Registered Nurse – Adult; Nurse Independent / Supplementary Prescriber (V300)
Academic Qualifications: BSC (Hons) Adult Nursing practice, Research Methodology module (masters level), Principles of physical assessment module, independent and supplementary prescribing module (masters level).
Relevant Additional Training: Advanced communication skills training. The Oxford Advanced Course in Pain and Symptom Management (Sobell Study Centre). Level 2 Psychological Support Training. Leadership course. CISM course.
Professional Career: Nicola trained in Shropshire and has worked in a number of different trusts as a Staff Nurse on a surgical ward and in an Accident and Emergency department before starting her career as a Specialist Palliative Care Nurse. Nicola joined the Palliative Care Team at UHNM in August 2014.
Dani Jervis– Macmillan Palliative Care Nurse Practitioner
Professional Qualifications: Dip HE Adult Nursing, BSc (Hons) Clinical Practice, Nurse Independent / Supplementary Prescriber Non- medical (V300)
Academic Qualifications: Mentorship, Health assessment.
Relevant Additional Training: Sage and Thyme Facilitator, Advanced communication skills training.
Professional Career: Dani trained at Keele University and qualified in 2008. Dani started her career on an acute Diabetes and Endocrine ward where she had experience in the roles of acting deputy ward manager and SSNQ. Dani has always had a keen interest in Palliative care and was the Palliative Care Clinical Champion on the ward for a number of years. In July 2014 Dani joined the Palliative care Team for a 6 month secondment as the AMBER care bundle facilitator and in June 2015 took a permanent position within the team as a CNS where she had a dual role of education/teaching and clinical practice and aims to further develop her knowledge and skills in Palliative Care. Then in April 2019 Dani was appointed as Macmillan Palliative Care Nurse Practitioner within the team. Since then Dani has completed a Degree in Clinical practice which also included modules of Health assessment and Non-medical Independent/Supplementary Prescribing.
Charlotte Scott- Macmillan Specialist Palliative Care Nurse
Professional Qualifications: Bsc (Hons) Adult Nursing
Academic Qualifications: Core Themes in Palliative Care (Level 4) module, Specialist Palliative Role Development (level 4) module, Head and neck cancer care (level 5) module, Supporting & assessment in practice (level 4) module, Advanced communication skills (level 5) module
Relevant Additional Training: Chemotherapy administration, SAGE &THYME
Professional Career: Post qualifying Charlotte spent 3 years working on a general medical ward at Wigan Infirmary as a band 5 staff nurse; developing an interest in nursing oncology patients and specifically patients with palliative needs therefore she pursued this interest by working as a staff nurse at The Christie Hospital in Manchester. The Christie provided excellent experience in nursing oncology and palliative patients. For personal reasons Charlotte moved to London and spent 9 years at Bart’s health NHS trust, initially as a band 5 and 6 nurse on various oncology wards, developing experience managing complex palliative patients and managerial skills. She was successful in gaining a 12 month secondment with the hospital palliative care team which was made into a permanent band 7 post. For personal reasons Charlotte moved to Stoke and wanting to pursue her career in Palliative Care she joined to team in October 2016.
Fiona Read - Macmillan Specialist Palliative Care Nurse
Professional Qualifications: Bsc Adult Nursing. NMC Registered Teacher Qualification. Post Graduate Certificate in Higher Education.
Academic Qualifications: Level 6 Foundations in Stoma Care. Level 6 Paediatric stoma and continence care module. Level 6 Mentorship training qualification.
Relevant Additional Training: Advanced Communication Skills. Attended study day on mind, body breath integration.
Professional Career:
Fiona completed her nursing studies at keele University and during her time spent 3 months on an elective placement in Turkey. On qualifying, she worked as a staff nurse on a specialist hepatology and gastroenterology ward. After 12 months she progressed to joining the specialist bowel care team in surgery as a stoma care nurse. Fiona developed in the post and became a clinical nurse specialist in colorectal cancer, whilst also having a quality role in the team. With an interest in Education, Fiona took up a post for 2 years as a teaching fellow at Keele University, educating under graduate student nurses and running specialised post-graduate modules, for level 6 infection prevention and control and level 6 & 7gastroenteroloy modules. Wanting to return to clinical practice, Fiona then spent 5 months working at our local hospice, DMH and then returned to UHNM as a palliative care nurse specialist. She also has a quality role for the team. She has an interest in psychological support, communication skills, education, research and keen to explore ethical decision making in palliative care. She is currently undertaking her masters in Medical Ethic’s in palliative care. She also has an interest in yoga for advanced illness, loss grief and bereavement, undertaking her yoga teacher training presently.
Clare Darlington - Macmillan Specialist Palliative Care Nurse
Professional Qualifications: Registered General Nurse
Academic Qualifications: BSc (Hons) Advanced Professional Studies for Nurses, Midwifery and Health Visiting. Degree level modules: Specialist Palliative Care – Pain & Symptom Control module, Counselling & Communication module. ENB249 - Cardiothoracic Course. Diploma level modules: DC5 - Communication Course, DLE1 - Learning from Experience: Reflection on Practice and Portfolio Development
Relevant Additional Training: Psychological Support Level 2, National Advanced Communication Skills Training Programme (ACST), Leading an Empowered Organisation LEO Course (National Leadership Centre)
Professional Career: Clare completed her nurse training in Nottingham in 1991 and worked in Cardiothoracic surgery in at Nottingham City Hospital and The Royal Brompton Heart and Lung Hospital where she completed further specialist training. She returned to Nottingham and worked in various posts in the Cardiothoracic Unit at Nottingham City Hospital providing direct care for patients on the ward and subsequently as a Cardiac Rehabilitation Nurse and Clinical Educator developing an interest in support and education for both patients, their families and health care professionals. In 2004 Clare became a Lung Cancer Nurse Specialist, caring for patients with Lung cancer, supporting them throughout the pathway from pre-diagnosis, diagnosis, treatment and supportive care. Enabling Clare to be involved in projects both locally and nationally. This allowed her to develop a keen interest in palliative care and ultimately resulting in her moving to Stoke on Trent in Jan 2019 to join the Palliative Care team at UHNM.
Maggie Hogan- Macmillan Specialist Palliative Care Nurse
Professional Qualifications: Registered General Nurse
Academic Qualifications: Dip HE Adult Nursing and BSc (Hons) Adult Nursing
Relevant Additional Training: Mentorship course, sign off mentor, Foundations in palliative care course (St Christopher’s Hospice)
Professional Career: Maggie completed her training at Keele University in 2003 and worked on the Neurology ward as a staff nurse at Stoke for seven years, following this Maggie went on to work in the Dermatology department as a staff nurse. In 2010 Maggie moved back to London and worked as a community staff nurse, where she developed an interest in palliative care. Following on from this Maggie worked as Staff nurse at The National Hospital for Neurology and Neurosurgery. In 2012 Maggie started Working at St Christopher’s Hospice as a Staff Nurse, during her time at the hospice she became a deputy ward manager and later on the Discharge Coordinator. In April 2019 Maggie joined the palliative care team at UHNS.
Charmaine Butcher – Macmillan Palliative Care Nurse Practitioner and End of Life Lead Nurse
Professional Qualifications: BSc (Hons) Registered Nurse- Adult Nursing
Academic Qualifications: BSc Adult Nursing, Level 7 Postgraduate in Critical Care practice, clinical effectiveness and clinical practice; Nurse Independent / Supplementary Prescriber Non- medical prescribing (2022); Health Assessment in Clinical Practice (2022)
Relevant Additional Training: Advanced Communication Training, CISM Training, Introduction to CBT.
Professional Career: Charmaine did her training at Chester University and Leighton Hospital. During her time at Leighton she was involved in multiple quality improvements to help improve the care for patients and families in the hospital. Upon qualifying she worked in Critical Care at Stoke for nearly 4 years. During this time, she was able to do additional training to work alongside the organ donation team and be an on-call organ donation nurse. Charmaine’s passion in critical care was caring for palliative patients and making a difference to their families. She enjoyed the teaching side to role and would mentor students and new nurses. Wanting to pursue a career in palliative care she joined the team as an End-of-Life Care Facilitator/Macmillan Specialist Palliative Nurse. This role allows her to focus on education and research for the Trust but remain in a clinical role. In September 2020 she was successful in becoming a nurse practitioner in the palliative care team. Academically in 2018 she completed her post graduate certificate at Keele University in Critical Care Practice. She started the Advance Clinical Practice course at Keele University in 2020 and this is due for completion in 2023. Charmaine is interested in education, research, communication skills, and ethical decisions in palliative care.
Milly Cantre - Macmillan Specialist Palliative Care Nurse Practitioner
Professional Qualifications: Registered Nurse – Adult Nursing, Nurse Independent / Supplementary Prescriber (V300)
Academic Qualifications: BS Psychology, BS Nursing, BSc Hons Clinical Practice
Relevant Additional Training: Foundations of Palliative Care- Marie Curie, Advanced Communication Skills Training, Nurse Independent/Supplementary Prescribing
Professional Career: Milly worked as a staff nurse at Marie Curie Hospice in London following completion of the Overseas Nurses programme in 2011. Milly completed her mentorship module whilst working at the hospice as a junior ward sister. Since moving to Stoke-on-Trent in 2016, Milly has worked different roles in various organisations in the community. She briefly worked as the NANS Palliative care co-ordinator for SSOTP Palliative care coordination centre and as a unit manager in a nursing home. Milly has also worked as a Senior Staff Nurse at Douglas Macmillan Hospice. Milly joined the team in 2019 and has since completed her BSc Hons in Clinical Practice degree and Non-Medical Prescribing qualification.
Martha Chatfield - Macmillan Specialist Palliative Care Nurse
Professional Qualifications: Registered General Nurse, Non-medical Prescribing qualification, Acute Care BSc (Hons) Adult Nursing (1st) 2021
Academic Qualifications: Dip HE Adult Nursing, 1st BSc Hons Clinical Practice (Acute Care)
Relevant Additional Training: Mentorship course, Holistic Health assessment, advanced communication.
Professional Career: Martha completed her diploma in nursing at Keele University in 2013, going on to work on the Acute Lung Unit (ward 222/Non-invasive Ventilation Unit) for five years. While there she developed her role, working initially as a staff nurse as part of their nurse-led team, eventually going on to be a band 6 Senior Nurse on the unit. Whilst there she started her degree pathway in Acute Care, including her Mentorship, Holistic Health Assessment and dissertation modules. This is where Martha also began to develop her interest in palliative care, nursing many patients with end stage conditions, such as COPD, pulmonary fibrosis, MND and Lung cancer. She began to develop palliative skills, learning to manage breathlessness, anxiety, terminal agitation and other end of life symptoms. Also developing her communication skills; with difficult conversations and breaking bad news. Following this Martha worked for 2 years at Severn Hospice, in Telford, on the inpatient ward, taking a break from her degree studies but working on increasing her palliative knowledge and skills in a specialised palliative area. Martha joined the UHNM Specialist Palliative Care team in 2019 due to her interest in improving end of life care within the acute setting and has since completed her acute care degree with a first, including the non-medical prescribing module in 2021.
Rebecca Hill - Macmillan Specialist Palliative Care Nurse
Professional Qualifications: BSc (Hons) Registered Nurse- Adult Nursing.
Academic Qualifications: BSc Adult Nursing.
Relevant additional training: Essentials in Palliative and End of Life Care (The Christie School of Oncology), End of Life Care for All (e-ELCA), Practice Supervisor Training (Keele University), Pain and Symptom management for end of life and palliative care (Macmillan Cancer Support), Loss, grief and bereavement (Macmillan Cancer Support), Sage and Thyme Foundation Level, Mesothelioma and Emphysema Workshop.
Professional Career: Becky qualified from Keele University in 2017, since then she has worked as a Staff Nurse on Ward 223 for three years, which specialises in Cardiothoracic Surgery. During that time, she gained specialised knowledge on how to care for patient’s pre and post-surgery. This was developed further during a rotational post to cardiothoracic critical care where she looked after level 1 and 2 patients who required intensive nursing care. Becky has always had a passion for palliative care prior to qualifying and has always wanted to pursue a career in this area of nursing. Becky is planning to start her Health assessment in Clinical Practice module at level 7 in March 2022, with the hope to go on to her non-medical prescribing afterwards.
Giannina Davies- Macmillan Specialist Palliative Care Nurse
Professional Qualifications: BSc (Hons) Registered Nurse- Adult Nursing.
Academic Qualifications: BSc Adult Nursing.
Relevant additional training: Practice Supervisor Training (Keele University), Enhanced Level 1 Education Programme
Professional Career: Nina qualified from Keele University in 2015, since then has worked as a staff nurse on ENT and specialised surgical ward completing tracheostomy training and gained skills and knowledge regarding Head and Neck cancer. She then moved onto cardiothoracic ward nursing patient’s pre and post-surgery. After this she moved as a band 6 Quality Nurse to the escalation ward, gaining managerial experience and charging a busy medical ward. This background of surgery and medicine allowed development in palliative skills and learning. Nina has undertaken her Advanced Communication Training while with the team and currently ongoing with her Health assessment in Clinical Practice module at level 7, with the hope to go on to complete non-medical prescribing afterwards.
Jemma Courts – Administration Assistant- Palliative care Team
Qualifications: Medical Administration Diploma Level 2
Career: Jemma has worked in administration in the health sector, previously working within the community care equipment sector whilst completing her medical administration Diploma Level 2. The Diploma consisted of working in the NHS and Medical Terminology. In 2019, Jemma started a Health and Science Degree at the Open University completing the first year. Jemma continues with the second year of her degree, studying Psychology. Jemma’s role in the Palliative care team is to provide support with the administration duties, working alongside the palliative care team.
Palliative care aims to improve the quality of life of people affected by serious, life-limiting illness by paying attention to physical, psychological, social and spiritual concerns. The concerns and needs of family members and carers are also taken into account.
Palliative care is provided to patients in all areas of the hospital by a variety of generalist and specialist teams, and all clinical staff can seek advice and support from the Hospital Palliative Care Team for any patient
The palliative care team gives specialist care and information to people facing serious life limiting illness. We recognise that emotional, spiritual, family and financial worries might be just as important to you as physical problems. We work closely with the hospital doctors and nurses to support you, your partner, family and friends. We will usually see you on the hospital ward.
Who is in the palliative care team?
- We are a team of doctors and nurses who have taken specialist training in palliative care
- We work closely with other teams in the hospital who may be involved in supporting you
- We work closely with community services including GPs, district nurses and community palliative care team as well as local hospices
How can we help you?
We aim to:
- Offer you advice about managing pain and other physical symptoms
- Support you while you are facing serious life-limiting illness
- Offer support to those close to you
- Help you to plan for future care
- Offer guidance to the team who are planning your discharge from hospital
- Refer you to other services that might be helpful to you such as Occupational Therapists, discharge team and chaplains
- Offer practical suggestions to help you do the things that are important to you
Palliative Care unit on Ward 12
Some patients will benefit from a greater level of specialist palliative care and at County Hospital this can be provided in the palliative care unit located on Ward 12.
Visits are normally made between 09:00 – 17:00 Monday to Friday
(An emergency service is available on Saturdays and Sundays)
All messages/enquiries can be left for Royal Stoke and County Hospital sites on:
01782 674029 (24 hour answer phone)
You can write to us at:
Hospital Palliative Care Team C/O Outpatients 3
Royal Stoke University Hospital
University Hospitals of North Midlands NHS Trust
Stoke-on-Trent ST4 6QG
Advice is available out-of-hours and at weekends through the Douglas Macmillan Hospice Advice Line for individuals with palliative care needs in Staffordshire.
This service is available on 01782 344 300
What is end of life care?
The term 'end of life care' refers to the care people receive in the last twelve months. End of life care looks at the physical, emotional, social and spiritual aspects of care and will be adapted to a person's needs.
Who provides end of life care?
A number of health and social care professionals may be involved in the care being given at end of life depending on the person's needs. Examples may include hospital doctors and nurses, GP, community nurses, counsellors, chaplains (of all faiths or none), social workers, occupational therapists and complementary therapists.
Support
If you have a life-limiting condition or are caring for someone who does and you would like more information about the support available locally, please contact your GP, specialist nurse (if you have one) or any of the healthcare professionals involved in your care.
Planning ahead
If you have a life-limiting illness, or are approaching the end of your life, you may wish to make plans for your future care. Planning ahead can help you receive the care that you would like. This information could also be helpful to your family and friends.
What is an Advance Care Plan?
An advance care plan is a written statement that sets down your preferences, wishes, beliefs and values regarding your future care. An advance statement is not legally binding, but anyone who is making decisions about your care must take it into account.
Examples of preferences could include wishes regarding preferred place of care, wishes regarding tissue donation, wishes regarding spiritual care and personal likes and/or dislikes.
What does lasting power of attorney mean?
There are two types of LPA ( Health and welfare and Property and Finance ). You can find more information on the government website https://www.gov.uk/power-of-attorney
If you become unable to make decisions for yourself in the future, someone will need to make decisions for you. Generally, professionals will make decisions about your health and social care, and your family or carers will decide on day-to-day matters. If you wish, you can officially appoint someone you trust to make decisions for you. This is called making a lasting power of attorney (LPA).
What is a ReSPECT document
A ReSPECT ( Recommended Summary Plan for Emergency Care and Treatment ) document is an alternative process for discussing, making and recording recommendations about future emergency care and treatment, including CPR. It encourages people to plan ahead for their care and treatment in a future emergency where they may be unable to make decisions, however it is not a legally-binding document. You can find more information on http://www.uhnm.nhs.uk/our-services/respect/
What is the Purple Bow Scheme?
The Purple Bow is a charity funded initiative aimed at improving communication between staff and relatives. This works by having a bow displayed on room doors and curtains on a bay to indicate to staff that a patient is approaching last days of life. The main focus of the Purple bow is to help individualise the care provided to the patients who are in the last days of their lives. This forms part of the individualised care bundle for last days of life.
Car Parking
An 'exemption from car parking charges' permit is provided to relatives of patients under the Purple Bow scheme. If you would like further information about this please speak with a member of staff.
Open visiting for relatives and close friends
Open visiting is often permitted for relatives and close friends of patients under the Purple Bow scheme. This can be authorised by the nurse-in-charge.
The Carers Hub is a commissioned service by Staffordshire County Council and Stoke-on-Trent City Council to provide support to adults and young carers. To read more about the support services they offer please click the link> https://www.thecarershub.co.uk/
Breathlessness Patient Leaflet
Syringe Driver (Information for patients and visitors leaflet)
Palliative Care Cardiopulmonary Resuscitation (Information for patients and visitors leaflet)
Coping with dying Purple Bow (Information for patients and visitors)
UHNM Palliative Care Conference 2024 - This event is now fully booked.
19th March 2024
08:30- 17:00
Port Vale Football Club
Hamil Rd. Burslem
Stoke-on- Trent
ST6 1AW
Hospices & Staffordshire and Stoke-on-Trent Integrated Care Board (ICB) advice line - 0300 561 2900
