Here is some information on the types of surgery that we perform, as well as standard information leaflets
Sleeve Gastrectomy
Laparoscopic Roux Y Gastric bypass
Patient Information
What is Obesity?
Obesity is a condition where a person stores extra fat, this fat can affect a person’s health. People store extra energy eaten in their diet as fat.
Health risks of obesity include:
- Diabetes
- High blood pressure
- Sleep apnoea
- Depression
- High Cholesterol
- Heart Failure
- Gallstones
- Gastro-oesophageal reflux disease
- Infertility
(Health risks increase with BMI)
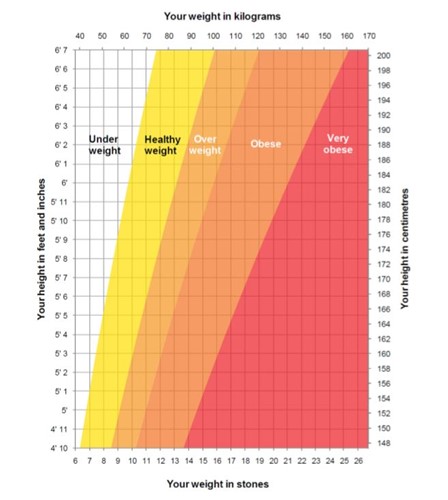
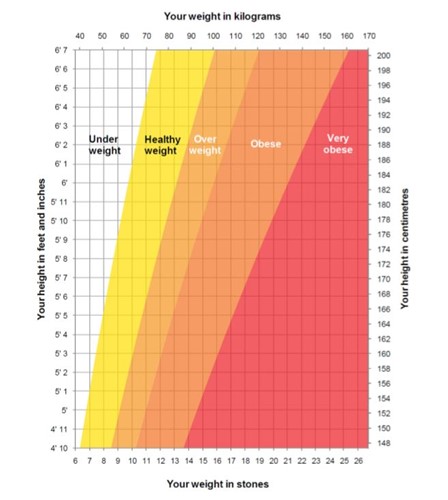
What is BMI?
Body Mass Index (BMI) is a measure of whether you are a healthy weight for your height.
BMI Classifications
Under 20:Underweight
20-25: Normal weight
25-30: Overweight
30-35: Obese, class I
35-40: Obese, class II
40+ Morbidly obese, class III
The BMI calculation is weight(kg)
height(m) x height(m)
kg = kilograms
m = metres
BMI Chart
What is weight loss (Bariatric) surgery?
Bariatric surgery is a group of operations designed to limit and restrict the amount of food you eat, some procedures will also reduce the amount you absorb from the food you eat.
The amount of food that you can eat will be greatly reduced, and you will feel fuller for longer. By eating fewer calories (energy) than your body needs, you will lose weight.
Bariatric operations are not an easy option and require you to change your lifestyle – you will need to eat healthily and sensibly and to do regular exercise after your operation. It is still possible to put weight on after these operations if you do not change your lifestyle appropriately.
It is important that you discuss your options for Bariatric surgery through with the surgeon and the team. Make sure that you ask questions if you are unsure of anything. Sometimes it helps to write your questions down before your appointment, so that you don’t forget to ask anything.
Potential side-effects after surgery
Dumping syndrome – most commonly occurs after the Gastric bypass operation. Food moves from your new stomach into the top of the small intestine more quickly than it used to. If the diet is too high in fat or sugars, the meal can move through very quickly, which causes discomfort – you might feel sick, dizzy, faint, sweaty, hot/cold, clammy. It is important to avoid high sugar and high fat foods, both to prevent dumping syndrome and to ensure a low calorie diet.
Vomiting – you should not expect to vomit after surgery. You may vomit if you overeat, therefore stop eating as soon as you feel full. Other ways to avoid problems are to take time over meals, sit up straight whilst eating, and to chew food well.
Constipation – ensure you drink at least 2 litres of fluid per day and that you have a good intake of high fibre foods such as wholegrain cereals, fruit and vegetables. Discuss with your GP if constipation remains a problem.
Diarrhoea – some people may experience looser stools after surgery, this is due to the food moving through your digestive system more quickly. Some people may get diarrhoea after eating fatty foods.
Hair loss – some people experience hair loss, especially if they lose a lot of weight very quickly. Ensure you are eating a healthy, balanced diet and hair loss should stop over time.
Loose skin – it is possible that you will be left with loose skin after losing significant amounts of weight. Plastic surgery can be considered and would be recommended two years after weight loss surgery, once weight has stabilised. Referral to the plastic surgeons is not part of the Bariatric package, and a separate referral from your GP would be required.
Vitamin and Mineral deficiencies – in some patients we notice vitamin and mineral deficiencies. Your blood levels will be checked at six monthly intervals to monitor this, and recommendations will be made. You are less likely to develop a vitamin or mineral deficiency if you follow a healthy, balanced diet, and take your vitamin and mineral supplements as advised by the team.
Development of Gall stones that may require surgery if causing problems at a later date.
Bariatric surgical procedure
At University Hospital of North Midlands, Bariatric surgery is routinely carried out laparoscopically (keyhole).
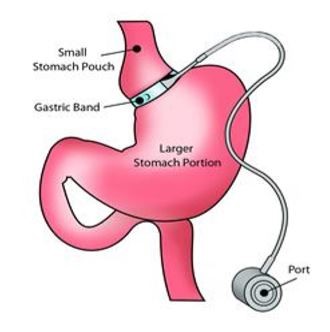
Laparoscopic Gastric Banding (NOT DONE AT UHNM)
This is a restrictive procedure where a ‘band’ is placed around the top of the stomach to create a small pouch where food enters. Food then exits this pouch slowly through a small passageway left by the band and passes into the larger part of the stomach and digestion continues on as it would normally.
As the top stomach pouch is only very small, it gets filled up quickly, giving you a feeling of fullness very quickly, and therefore reduces the amount you eat, helping you to lose weight.
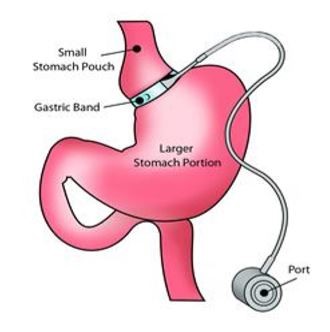
You might expect to lose an average of 40-50% excess weight after a Gastric band.
This procedure of gastric banding is not done in our hospital as we uniformly feel that there are better options available offering better outcomes (as below) and there are complications with the band that may necessitate it’s removal.
The team at UHNM however have a good experience in removing gastric bands done elsewhere due to complications.
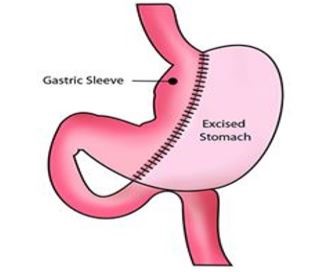
Laparoscopic Sleeve Gastrectomy
This operation is performed using a key hole technique making five small cuts, it is performed under general anaesthetic, and requires a hospital stay of usually two nights.
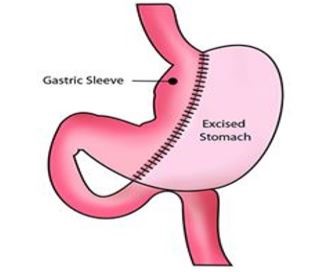
A Sleeve Gastrectomy is an operation that reduces the size of the stomach by around 75%. It reduces a person’s appetite and the amount of food they can eat, and therefore results in weight loss.
The operation involves part of the stomach being removed, leaving a smaller stomach in the shape of a ‘sleeve’. Food will leave the stomach as normal through the pyloric valve at the bottom of the stomach and go into the small intestine. Therefore, although the stomach is smaller, the way it works remains unchanged.
Sleeve Gastrectomy can be considered as the first part of a two stage process. An initial Sleeve Gastrectomy, followed at a later date by either a Gastric Bypass or by a Duodenal Switch.
Gastric Bypass and Duodenal Switch are both complex operations, and where super obese patients have severe weight related complications, these complex operations may be too risky to proceed with, therefore a Sleeve Gastrectomy is considered as an initial treatment.
![]()
You might expect to lose an average of 60-70% excess body weight after a Sleeve Gastrectomy .
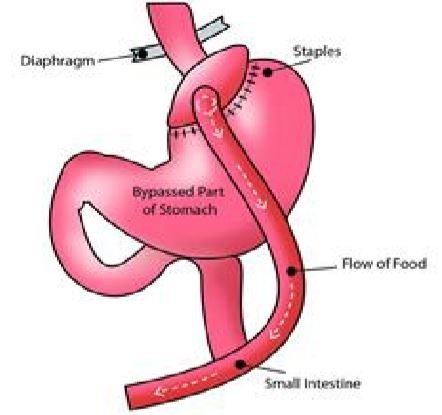
Laparoscopic Roux Y Gastric bypass (RYGB) – Standard Bypass
A small pouch (about the size of an egg) where food enters is made at the top of the stomach. This pouch is detached from the larger, bottom part of the stomach.
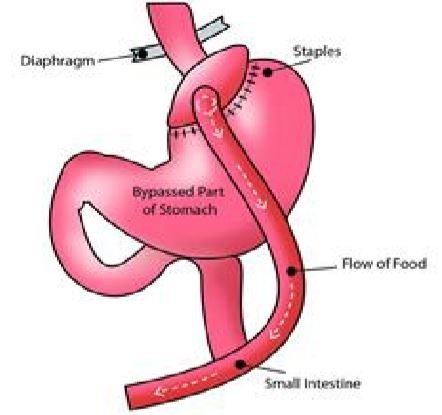
Part of the small intestine is then divided, and the bottom end is pulled up and attached to the small pouch, food goes into the small pouch and then straight into the small intestine.
The larger part of the stomach is still attached to the top part of the small intestine and the rest of the small intestine, allowing gastric juice to be drained through the gastro-intestinal system.
Gastric bypass works by reducing the amount of food you eat – the small pouch gets full quickly, making you feel full earlier. There is also a degree of malabsorption that occurs after the Gastric bypass, as the food you eat bypasses the first part of the small intestine.
![]()
You might expect to lose an average of 70-75% excess body weight after a Standard RYGB Gastric bypass.
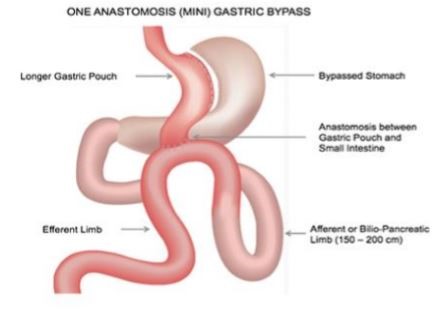
Laparoscopic One Anastomosis Gastric bypass – Mini Bypass
The “Mini bypass” as it is commonly known has been an increasingly used operation in the last 5 years or so.
This operation is similar to the standard bypass except for the following:
1) Longer stomach pouch ( to protect from reflux of bile and acid)
2) One join (only) between the stomach and the small intestine in comparison to the standard bypass where there are two joints (anastomoses).
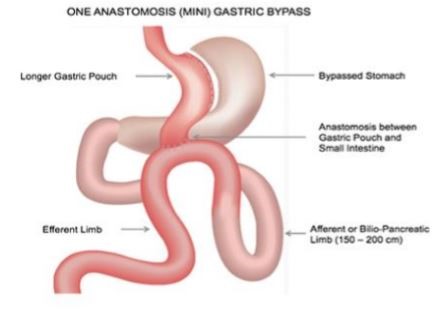
It is a simpler procedure and takes a shorter time to perform and gives the same amount of weight loss and improvement in other problems such as diabetes, hypertension, high cholesterol etc. However it is known to cause a higher incidence of anaemia and a potential to ongoing reflux of acid and bile. It is not generally offered in patients having symptoms of acid reflux. It is also known to cause occasional excess weight loss and diarrhoea which can be bothersome.
We do not routinely offer this operation as a standard procedure, but have this as a backup option if a standard bypass cannot be performed due to technical challenges at surgery.
The team at UHNM believe that the standard bypass is still the gold standard procedure which has stood the test of time ( > 50 years0 when it comes to a bypass and have been doing it safely over the years when it can be technically done .
However it can be offered to patients who specifically requests this surgery understanding the higher chance of reflux and the lack of long term follow up data in comparison to the standard bypass.
You might expect to lose an average of 70-75% excess body weight after a Mini bypass.
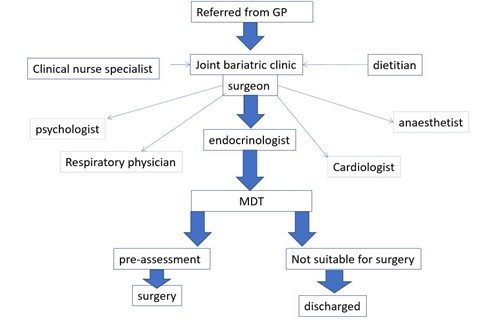
Weight loss surgery – the process
The Multi-disciplinary team (MDT)
You will be seen by a variety of Health Professionals before and after your operation. It is likely that you will be seen in a ‘Joint Bariatric’ clinic.
The Bariatric Multi-disciplinary team consists of: Surgeon, Endocrinologist, Specialist Nurse, Dietician, Anaesthetist and Psychologist.
You may be seen by other Consultants who usually look after other aspects of your health, alongside the Bariatric process. These might include heart specialists, respiratory physicians and kidney specialists.
Please Note: If you fail to attend any out-patient appointments without calling to cancel the appointment, then you may be discharged from the Bariatric service.
Weight loss before surgery.
At your first clinic visit, it is likely that the Consultant will give you a target weight to achieve. Typically, this is around 10% of your weight recorded at your clinic visit. There are two reasons for this;
1. Liver shrinkage: weight loss will help to reduce the size of your liver down. The liver holds excess energy, by sticking to a strict, calorie controlled diet, you will help to use this energy up, and reduce the size of your liver. This is important, as the liver lies in front of the stomach, meaning that the bigger the liver, the harder it is to gain access to the stomach, which is important for surgery. The more weight you can lose safely before your operation, the easier it is for your surgeon to gain access to your stomach, and therefore the safer the procedure will be.
2. It is important that you make healthy lifestyle changes before your weight loss operation, as you will need to make healthy lifestyle changes long term in order to keep your weight controlled.
You will not be offered surgery until you have reached your target weight. The team will support you to lose your weight.
You will also be given a ‘Liver Shrinking’ diet to follow for the two weeks before your operation – this ensures that the Liver is shrunk down as much as possible, and it is important that you keep to this diet.
Pre-assessment
As the time of your operation draws near, you will be asked to attend a Pre-assessment appointment.
The nurse will check:
- Medical history
- Medications
- Weight, height and BMI
- Blood tests
- ECG, Chest X-ray and other tests as necessary, such as Echocardiogram
You may be seen separately by the anaesthetist if necessary.
Smoking
If you are a smoker you will be required to completely stop smoking prior 6 weeks to surgery and continue not to smoke after surgery.
You will be tested if you are continuing to smoke (urine and breath tests) prior to surgery and will not be offered an operation if you are found to be smoking. Patients have had their surgery cancelled on the day of surgery when they have found to continue smoking.
Day of Surgery
You will be asked to come into the ward early in the morning on the day of your operation, and you should not have eaten anything from 12 o’clock the night before. You should only have had a clear drink up to 7 o’clock that morning, and then you will be Nil by mouth.
After surgery
You will be allowed to drink 30mls of water per hour on the day of surgery. You will be mobilised on the ward six hours after surgery.
On the day after surgery (day 1), you will be able to drink free fluids as tolerated. You will be free to mobilise on the ward.
On day 2, you will be allowed drinks as tolerated and liquid diet. You are usually discharged home on day 2.
You will progress from liquid diet to solid diet over a period of 8 weeks; your dietician will discuss this with you in more detail before you go home. Below is a basic idea of what to expect.
- Weeks 1-2 Liquids only
- Weeks 3-6 Liquidised/Blended/Pureed diet
- Week 7 Soft Diet
- Week’s 8+ Normal diet.
Diet and Lifestyle changes long term
Any obesity surgery should be seen as a tool to help you lose weight. It is important that you make healthy diet and lifestyle changes long term to keep the weight off. Without lifestyle changes, it is possible to put weight back on, even after surgery.
We perform the surgery- You make it work!
- You will be asked to eat a healthy, well balanced diet, and to ensure regular physical activity. Your dietitian will talk through your diet with you on a regular basis.
- Eat a regular, well balanced diet, and eat three meals per day.
- Include 2 protein containing meals per day – protein is found in meat, fish, eggs, beans and pulses.
- Eat plenty of fruit and vegetables.
- Avoid foods with a high sugar or fat value.
- Drink plenty to avoid dehydration, aiming for 8 cups of fluid per day. Try to drink separately to meals.
- Alcohol is best avoided in the first 2 months after surgery. After gastric surgery, alcohol is more quickly absorbed into the body, which is worth bearing in mind. In addition, alcohol does contain calories, so intake needs to be sensible in terms of weight management.
- Eat slowly and chew food well. Stop eating when you feel full, eating when you feel full can lead to nausea and vomiting, and your stomach size may stretch.
You will be advised to take a multivitamin and mineral supplement, to ensure that you are still consuming all the vitamins and minerals you need. Your dietitian can advise you if you are unsure. The regular “4 for life” which include multivitamins tablets, iron tablets, vitamin D and B12 injections ( once in 3 months) are to be religiously taken to avoid nutritional problems in the long term.
Follow-up
It is important that you commit to long-term follow up after your procedure. You will be followed up by the Bariatric team for 2 years after your operation. After this, you should have your blood levels checked at your GP every six months.
You will be followed up in the Joint clinic 6-8 weeks after your operation. You may be seen by the dietitian before this.
Helpful contact details
Mr N Balaji, Consultant (Clinical lead for Bariatric surgery ), Secretary 01782 679876
Mr C V N Cheruvu, Consultant (Surgeon), Secretary 01782 679876
Mr V S Rao, Consultant (Surgeon), Secretary 01782 679876
Mr Sharples Consultant (Surgeon), Secretary 01782 679876
Mt Tzvetkov Consultant (Surgeon), Secretary 01782 679876
Kate Brandrick (Bariatric Dietician)
Emily Cooper (Lead Bariatric Dietician) 01782 676050
Emma Turner (Bariatric Dietician)
Dietitian email: Bariatric.dietitian@uhns.nhs.uk
Lynn Bedson (Bariatric Nurse Specialist) (01782) 671670
Bridie Cornes (Lead Bariatric nurse specialist) (01782) 679896
Ngozi Etumnu (Bariatric Nurse Specialist) (01782) 672977
Nurse email: bariatric.services@uhns.nhs.uk
Please contact the bariatric secretarial team on (01782) 679876 for all consultant clinic appointment queries.
Please contact the Dietitians for all dietary issues.
Please contact the Bariatric Nurse Specialists for all other bariatric issues
Please Note: Please call a member of the team on the above numbers with any concerns or issues.
Useful Websites:
• Attend Patient Information session To establish if you wish to pursue with Bariatric Surgery
If you failed to attend an appointment you will not be listed for Surgery or you could be discharged from the pathway.
• Standard pre-op care-NBM, consent, anti-embolic stockings, who check list etc.
• Named nurse to make follow up calls usually 1 day/1 week/1 month post discharge but depends of day of discharge
• Clinical review every 4-6 months-clinics are either by consultant, consultant telephone or nurse led for 2 years post surgery
Your surgeon may ask you to have a strict milk and yogurt diet 2 weeks before your weight loss operation.
This diet will help to shrink your liver and lose weight so that your surgeon can operate much more easily. Losing weight before your operation will also reduce your anaesthetic risk.
If you have diabetes the calorie restriction may require a reduction in your diabetes medication, please contact your health care provider or the diabetes nurses team at UHNM on 01782222969.
- Water, tea (no sugar), coffee (no sugar), still diet drinks, low calorie squash, clear soup such as consommé (clear beef soup), Oxo or Bovril.
- Take an A-Z/complete multivitamin and mineral supplement. If you need more advice ask your dietitian or surgeon.
- Aim to drink 2 litres of allowed fluids daily to prevent constipation. You can take a nonbulking agent such as Lactulose obtained from your doctor or pharmacy.
- After your operation follow the diet plan given to you by your dietitian.
- Useful Websites: www.bospa.org www.WLSinfo.co.uk www.nice.org.uk/CG43
Remember that the surgery is a tool and you must work hard after surgery to change your lifestyle to become and stay healthy.
❏ I understand and agree to the preoperative attendance policy.
If you fail to attend two or more preoperative appointments (including medical, endocrine, dietician, nursing and psychology appointments) then you will be discharged from the bariatric programme without further notice
We understand that appointments do on occasions need to be rearranged, however we expect you to be committed to attending appointments and therefore if an excessive number of appointments (in most circumstances greater than four) are cancelled by yourself we will also discharge you from the programme.
In this situation your doctor will be unable to re-refer you for a period of one year.
❏ I agree to be committed to follow up care after surgery.
This includes both short-term and long-term care. We routinely expect to follow you up for two years after surgery. It is important that we monitor your weight as well as nutritional parameters, to avoid potential long-term complications.
❏ I agree to follow the dietary plan as advised by the dietetic team.
Failure to engage with the dietetic team may result in your discharge from the service. It is expected that completion of the pre-operative pathway should take no longer than 12 months and at this point your progress will be reviewed and a decision made by the multidisciplinary team as to whether you can continue or should be discharged from the service.
❏ I agree to take nutritional supplements regularly, as directed.
For most patients this will include a daily multivitamin, iron tablets and vitamin D tablets. We also recommend all patients have injections of vitamin B12 every three months. In some situations we may recommend additional supplements.
❏ I understand that I need to take responsibility for my weight management.
If you are having difficulties, you should contact our team for guidance and assistance. It is expected that completion of the pre-operative pathway should take no longer than 12 months and at this point your progress will be reviewed and a decision made by the multidisciplinary team as to whether you can continue or should be discharged from the service.
❏ I understand that I will not be offered surgery if I am smoking or using any nicotine products. I understand that smoking should never be started or resumed after bariatric surgery.
The effects of smoking can result in life threatening stomach bleeding, ulcers, perforation, gastrointestinal problems requiring emergency surgery, and/or potential death.
❏ I understand that it is not advisable to become pregnant during the next two years after bariatric surgery.
Pregnancy outcomes are very good after bariatric surgery but there are potential increased risks if you become pregnant within the first two years. Oral contraceptive methods are not effective after surgery and therefore other contraceptive methods should be discussed with your GP.
❏ I understand that it is inevitable that there will be excess/redundant skin secondary to weight loss after bariatric surgery and surgical treatment of the same is not offered in the NHS through the bariatric service.
❏ I agree to information (including my NHS number) about my care and progress being submitted anonymously to a national database managed by the British Obesity and Metabolic Surgery Society for quality improvement purposes.