Located just off the A34 on the ground floor in the Cancer Centre at the Royal Stoke University Hospital is the Radiotherapy Department where there are 4 Linear Accelerators, a superficial skin treatment unit, Brachytherapy treatment suite, a dedicated CT scanner, treatment planning suite & clinic areas.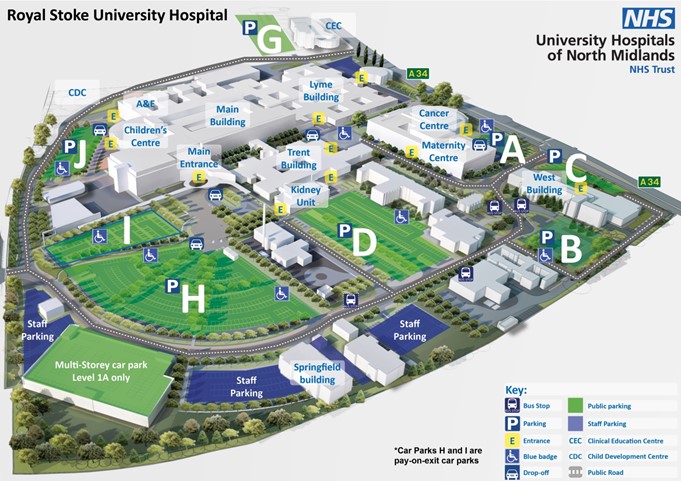 The closest patient car parks to the cancer centre are A, C & D. Patients will need to pay for parking for their first appointment; the ticket machines are located on each of the car parks. But then after that those people undergoing cancer treatment will be given a parking pass which will mean that they can park in any of the patient car parks on the hospital without having to pay, as long as the valid permit is displayed in their car.
The closest patient car parks to the cancer centre are A, C & D. Patients will need to pay for parking for their first appointment; the ticket machines are located on each of the car parks. But then after that those people undergoing cancer treatment will be given a parking pass which will mean that they can park in any of the patient car parks on the hospital without having to pay, as long as the valid permit is displayed in their car.
Radiotherapy
Radiotherapy is the use of carefully targeted high energy X-rays to treat patients with cancer. It damages the cancer cells and stops them dividing and growing. Normal healthy cells can also be damaged by Radiotherapy which causes treatment side effects however, healthy tissue can repair but cancer cells can’t. The treatment may be radical with the aim of curing the disease, or it may be palliative to control the symptoms and slow down the progression of the disease. The treatment is delivered by machines called linear accelerators. Each patient's radiotherapy treatment is individual and tailor-made for them.
Patients will be seen before attending the Radiotherapy Department by their Consultant Clinical Oncologist (Doctor) who will discuss different treatment options and help the patient to decide what the best treatment plan is for them. Radiotherapy can either be given on its own; or alongside surgery, chemotherapy or hormone therapy. The Doctor will go into detail about the treatment and any side effects that may happen and check that the patient is fully informed and happy to go ahead with the treatment.
All patients who are to receive radiotherapy will have their treatment carefully planned first. Most patients have a CT scan which is used to outline the areas to be treated. This will be slightly different than any previous scans that they may have had as they will be in a position specifically for the Radiotherapy treatment.
Some patients will be required to follow specific instructions before their planning scan and during their treatment; these should be detailed in the appointment letter which is sent to inform them of their date to attend for their CT planning scan. It is important to read these instructions carefully and follow them when attending the department. A member of staff will go through these with the patient in person to make sure they are fully aware of what to do.
The CT scan is very quick & painless; the patient will be positioned in a way that is comfortable for them but allows good access to the area to be treated and also to be secure enough to be accurately reproduced every day for when they come for treatment. Most patients will have some permanent tattoo marks placed on the skin. They are very small and no larger than a freckle. The tattoos are made with a small amount of ink and a small needle placed under the surface of the skin. The tattoo dots are permanent but they are very small and usually not very noticeable, they may fade slightly over time. These tattoo dots will enable the treatment staff to position the patient in the same position as they were for the CT scan on a daily basis for the Radiotherapy treatment. Patients having treatment in their head or neck region will not have tattoo marks and will instead have a specially constructed plastic shell, or mask, made for them to wear during each treatment for accuracy and to help keep the head perfectly still.

Radiotherapy treatments are routinely delivered every weekday Mon-Fri between 8.30AM-4.30PM. It is important that patients keep to their appointment schedules as much as possible, however if they are feeling unwell or unable to attend then they should contact their treatment machine directly, the telephone number can be found on the appointment card given to them at their CT scan or in the contacts section at the end of this page. Patients are advised to discuss any plans for holidays with their consultant or radiographer as soon as possible. In the Radiotherapy department at the Royal Stoke we do work most public bank holidays; we will make sure that people are aware of the dates that they need to attend. Some gaps in treatment may be allowed when machines are serviced, machines breakdown or during some public holidays. Any necessary adjustments will be made to treatment to account for these. Very occasionally we may ask patients to attend for treatment on a weekend but this will be made well aware to the people this may affect.
Radiotherapy is delivered by Linear Accelerators (Linacs). We have 2 different types of Linacs in the Radiotherapy Department at the Royal Stoke, with all 4 machines doing the same job and having state-of-the art up-to-date technology
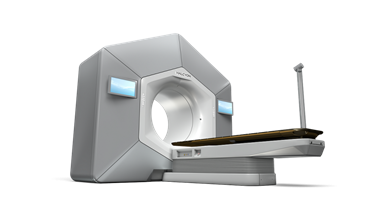
Halcyon treatment machine ©Varian 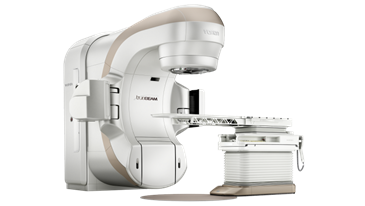 Truebeam treatment machine ©Varian
Truebeam treatment machine ©Varian


The number of treatments on the linac depends on each patient's condition. It can be anything from 1 to 37 treatments and each treatment can take anything from 5 to 60 minutes. Most of the time is taken in getting the patient in the right position for the treatment. The delivery of the treatment itself is similar to an x-ray and very quick & painless with nothing to see or feel. All we need the patient to do is keep very still and breathe normally.
No-one is allowed to be in the room while a patient is receiving radiotherapy, but the Therapy Radiographers can see and hear them at all times through CCTV & intercoms. The CCTV is never recorded; it is just a live feed so that the patient can alert the staff if needed. The machine can always be stopped if necessary and the staff can go into the room to attend to the person. The Radiotherapy Department at UHNM is a very busy unit, but wherever possible the staff do try to offer patients’ appointments at times of day that work around them in order for patients to make it easier to organise their lives around the treatment.
External radiotherapy does not make people radioactive so it is perfectly safe for people to be around others (including children) during and after their course of treatment. However it may be advisable to avoid being close to people who are unwell, especially if the patient has had/is having chemotherapy. It is also very important that patients are not and do not become pregnant during their course of radiotherapy. If anyone is concerned regarding this please discuss this with a member of staff.
Radiotherapy is delivered by a team of suitably trained radiographers, both male and female. We are also a teaching hospital and regularly have student radiographers in the department who are supervised by trained staff. Chaperones can be used if wanted; please make a member of staff aware if the patient would like this.
Patients have daily contact with the radiographers who look after them while they are attending for treatment and can answer most questions that they may have. During the course of treatment patients will also normally have the opportunity to speak to a nurse or a doctor about any other concerns or specific aspects of their care.
Before attending the radiotherapy department the patient will be seen by their Consultant Oncologist who will detail the area to be treated and any related side effects that may happen. They will advise how we may deal with any side effects and give the patient the opportunity to ask any questions they may have. Before their planning CT scan a radiographer will go through the side effects with them again to check that they have understood everything that was said in their first consultation and that they are still happy to go ahead.
Side effects will vary depending on what area of the body is being treated. Side effects are usually gradual and will build up over time during the treatment course. They are also very individual so can be difficult to predict, and each person may not experience the exact same effects as someone else having a similar treatment. If the patient or relatives have any concerns or would like any advice then please let the radiographers know. The staff are very approachable and will see the patient on a daily basis so are always available to ask questions to if there is anything that the patients are worried about.
The most common side effect for the majority of treatments is tiredness. Unfortunately not much can be done for this other than resting as much as needed, doing some light exercise if possible and drinking plenty of fluids. Other side effects depending on the area being treated can include skin soreness, hair loss (only in the area being treated), diarrhoea & nausea amongst others. The patient is welcome to speak to a Doctor or a member of the treatment team about what effects may be specific to them.
Once treatment is complete, short term side effects may continue for a few weeks even though the patient is no longer attending for treatment. This is very normal however if they have any concerns then they can still get in contact with the treatment team who will be able to advise further. If the patient has been given any advice regarding treatment side effects (i.e. medication, pain relief, and skin care) then please continue to carry on with this advice until the side effects have eased away.
Some patients may experience some long term side effects that can sometimes persist for several years. This will be explained in detail by the Oncologist before commencing treatment to make sure patients are fully aware of what to expect.
There are some very useful booklets available in the department or via www.macmillan.org.uk which explain the side effects relating to the different areas of the body that are being treated. Please make sure patients only take the information relating to their specific treatment area or there may be some side effects that do not relate to their specific situation. Radiotherapy only affects the area being treated so if they are having problems elsewhere on their body other than the treatment area they may be advised to get in contact with their GP.
Brachytherapy is only used for a few specific treatment sites and if appropriate it may be mentioned to the patient by their doctor. Brachytherapy is an internal treatment which uses a measured dose of radiation directly to the cancer site. Brachytherapy is delivered through applicators placed inside the body by a skilled doctor or therapy radiographer.
The treatment destroys cancer cells while doing as little harm as possible to normal cells and will not make the patient feel generally unwell. It does have some local side effects which will be explained to you when you are first seen.
If a patient is due to have Brachytherapy and would like further information please contact the Brachytherapy Team Tel: 01782 672529. (Mon-Fri: 8.30 – 5.00)
The superficial Xstrahl Gulmay machine treats superficial (close to the skin surface) cancers, mostly skin cancer, with low energy x-rays that do not travel deep into the body. This means that it is not invasive and there is very little tissue damage. Furthermore, it results in a better cosmetic outcome than surgery.

Firstly the consultant would mark the area to be treated on the patients skin and prescribe the treatment. The patient will then be seen by the Gulmay team who will take a photo and draw a template of the area to be treated thus ensuring accurate treatment. They will be given their treatment appointments giving the team time to prepare the treatment.

For treatment it might be necessary to place some shielding around the area to be treated and the machine will be moved into position gently resting on the skin. The treatment takes between 2 and 8 minutes and it may be necessary for several treatment sessions.
For any further information please contact the Gulmay team on 01782 672529 (Mon-Fri 8.30-4.30).

After radiotherapy has finished
Once treatment is complete, patients can still call the machine that they were treated on if concerned by any continuing side effects or for any further advice or reassurance. Most patients will have an end of treatment review appointment with either their Oncologist or the Radiotherapy Advanced Nurse Practitioner. This will be to see how they have got on with treatment overall and advise them of the next steps. This can either be face to face or by telephone. The treatment staff will tell the patient when this is going to be.
After this most patients will have a follow up appointment with their consultant, this can be anywhere from a few weeks to 3 months depending on the treatment area/how they have coped during the treatment. Some side effects can continue for an extended period of time so this will be an opportunity for patients to discuss this with their doctor. If an appointment letter has not been received a week or so before the patient is expecting an appointment then please get in touch with the Doctors secretary via switchboard or the Radiotherapy department who will look into this for them.
Radiotherapy reception 01782 672600
Radiotherapy scheduler 01782 672518
Radiotherapy CT scanner 01782 672516
T1 01782 672505
T2 01782 672506
H1 01782 672507
H2 01782 672508
Nurses base 01782 672522
Chemotherapy reception 01782 672500
Emergency Assessment Unit 01782 672444
Royal Stoke Hospital switchboard 01782 715444
https://www.nhs.uk/conditions/radiotherapy/
Cancer Support Services
- Macmillan Cancer Support and Information Centre@ UHNM (10AM-4PM) Tel: 01782 676333
- Macmillan support macmillan.org.uk Tel: 0808 808 0000
Useful leaflets & information: https://www.macmillan.org.uk/cancer-information-and-support/treatment/types-of-treatment/radiotherapy
- Dougie Mac Hospice Email: post@dmhospice.org.uk Tel: 01782 344300
- Patient Advice & Liaison Service (PALS) Office Tel: 01782 676450 or 676451
University Hospital of North Midlands
Newcastle Road
Stoke-on-Trent
Staffordshire
ST4 6QG
Email: complaints.department@uhnm.nhs.uk
Cancer research https://www.cancerresearchuk.org/about-cancer/cancer-in-general/treatment/radiotherapy

