We have a well-established service for video capsule endoscopy at County Hospital. We offer patency capsule, small bowel, colon and crohn’s capsules.
A capsule endoscopy is a procedure where a special capsule is swallowed that takes pictures as it travels through the gut. The images are recorded onto a monitor worn by the patient. The capsule is excreted and simply flushed away and the recorder returned to the hospital for analysis of the images.
The small bowel video capsules are used to investigate a part of the bowel that is not as easily visualised by conventional methods.
Colon capsules may be used as an alternate to colonoscopy in some cases. Capsule endoscopy is a less invasive, radiation-free day-case procedure.
Colon video capsule Endoscopy
What is a colon capsule?
This is where a special capsule containing a small camera, is swallowed allowing images of the bowel to be recorded as it travels through the gut.
Why do I need to prepare for this procedure?
Your bowel needs to be empty for the procedure so that the Doctor or Specialist Nurse can see the lining of your bowel.
To achieve this you will need to alter your diet for a few days before the procedure and take specific bowel preparations before the procedure.
The changes are explained in this leaflet.
What is bowel prep?
You have been supplied with an oral preparation which is a bowel cleansing agent (also referred to as “bowel prep”). This is called Moviprep®.
The purpose of this medication is to clear out your bowels and ensure safety and effectiveness of the planned procedure.
You may also require a recent blood test to check your kidney function.
What are the risks of Moviprep® ?
The person prescribing the Moviprep® will have assessed your risk and identified that the medication is appropriate for you.
The risks include:
- Developing dehydration.
- Low blood pressure
- Kidney problems.
- Taking Moviprep®
The following will apply when taking the bowel
preparation:
- The Moviprep® will cause diarrhoea and urgency so you will need to stay close to toilet facilities after you have taken it.
- If after taking both doses (all 4 sachets) of the Moviprep® you have not had your bowels open within 7-8 hours of the last
dose, please seek medical advice as soon as possible.
- Make sure that you drink plenty of water up to 2 hours before your procedure as the bowel prep can cause dehydration.
- Do not drink dark coloured liquids or milk. (refer to dietary information).
- If you experience symptoms of dizziness or light headiness (particularly on standing up), thirst or reduction in passing urine, then you may be dehydrated and should seek medical attention.
All bowel cleansing agents cause diarrhoea so if regular medication is required, it should be taken more than 1 hour or at least 1 hour after taking the Moviprep®.
Do not take any other medication at the same time as you are taking the bowel prep,
Moviprep® and other medication.
Please tell the Nursing Staff as soon as possible on the number at the end of the leaflet if you:
Take any medicines to thin the blood or to prevent blood from clotting (anticoagulants or antiplatelets, such as Warfarin, Rivaroxaban, Dalteparfin or Clopidogrel). If you only take low dose 75mg aspirin, you do not need to call.
Have diabetes (contact your Nurse Specialist).
Have an allergy to Moviprep® or its ingredients.
Please let us know if you are taking any regular medicines at your pre-assessment appointment (including anything you buy yourself over the counter or any herbal or homeopathic medicines).
The diarrhea caused by the bowel preparation can make the oral contraceptive pill less effective. You should continue to take your contraceptive pill as normal but extra precautions (such as condoms) must be used for 7 days after completing the bowel prep.
Refer to the manufacturer’s instructions when taking the Moviprep® for a list of ingredients and allergies.
There may be medicines which you are asked to stop taking and these include:
- Heart/Blood pressure tablets e.g. Lisinopril, Ramipril, Perindopril, Captopril, Losartan, Candesartan, Irbesartan, Valsaratan;
- Diuretics (Water tablets) e.g. Furosemide, Bendroflumthiazide, Spironolactone, Amiloride, Co-Amilfruse, Bumtanide, Metolazone, Indapamide, Eplerenone;
- Anti-inflammatory drugs, such as Ibuprofen, Naproxen.
- Tolvaptan: Used for progressive Autosomal Dominant Polycystic Kidney disease or conditions causing low sodium.
Your medication will have been discussed and advice given during your clinic or pre-assessment appointment.
Dietary Management – Low Residue Diet
Three to five days before your procedure you should start to eat a low residue (fibre) diet. This reduces the stool (poo) residue in the bowel.
The main sources of fibre in the diet are cereal products, vegetables, seeds and fruits, so these foods need to be reduced..
It is important to have regular meals and a varied diet which includes foods such as meat, poultry, fish, eggs and dairy products (milk, cheese, yoghurt)
It is important to drink plenty of fluid and at least 8-10 cups of water or squash per day (avoid red/purple coloured squash). This helps to flush the bowel contents out and will improve the effect of the bowel preparation. It will also prevent you from becoming dehydrated.
A vegan diet sheet is available from the Endoscopy Department if required. Please contact the number at the end of this page.
Suggested meals you can eat that are low residue
BREAKFAST
Cornflakes / Rice cereals
White bread toasted / egg
- (little butter)
(DO NOT EAT WHOLEGRAIN CERALS e.g. Weetabix,
LUNCH
Chicken soup with white bread/
Chicken or Ham sandwich/ Egg on white toast.
EVENING MEAL
White bread with ham /cheese (little butter) or boiled potatoes
(without skins) cauliflower, turnip
Small amount of chicken/white fish.
White rice/pasta
Food Choices you can eat
White bread or toast, pastry, plain naan bread and chapatti, crumpets. (made with white flour).
Cornflakes and rice breakfast cereals, but no bran, Marmite.
Soya or tofu, white rice, white pasta, and noodles, plain couscous
Do not eat lentils or pulses.
Cheese, cottage cheese
Biscuits made with white flour e.g. rich tea, shortbreads, plain cream crackers, arrowroot, plain scones.
Well cooked, lean (low fat) beef, lamb, ham, veal or pork, textured vegetable protein, Quorn®
Poultry, White Fish, Shellfish.
Eggs boiled or poached.
Dessert Choices you can eat
Sponge pudding and custard.
Mousses, plain or set yoghurts, cream.
Lemon Curd, Honey.
Bananas, canned pears, melon, stewed apple (Maximum of 2 portions per day)
Do not eat any seeds, pips, skins or piths
Orange, lime, lemon Jelly. DO NOT EAT RED/PURPLE JELLIES
ONLY the below fluids are allowed the day before your test.
Flavoured water/ Lemonade/ light coloured Squash, black tea/ black coffee, Oxo/ Bovril or other meat/veg extract cubes/clear strained soup e.g. consommé.
Boiled sweets and Jellies are allowed.
Flavoured water/ Lemonade/ light coloured Squash, black tea/ black coffee, Oxo/ Bovril or other meat/veg extract cubes/clear strained soup e.g. consommé.
Boiled sweets and Jellies are allowed.
Potatoes boiled or mashed without skins, sweet potatoes without skins boiled or mashed. Well cooked vegetables, turnip, squashes, carrots.
MOVIPREP INSTRUCTIONS
Five Days before the Test
Stop taking Iron tablets.
Three Days before the Test
Stop taking medications such ascodeine and loperamide and stool bulking agents such as fybogel, as these can reduce the effectiveness of the preparation.
If you suffer from constipation speak to your pharmacist or take your usual laxatives before you need to start drinking the Moviprep (do not exceed your maximum dose).
Three Days before the test
You should eat a low residue (low fibre) diet. This reduces the stool residue in the bowel.
The day before your test
NO more solid food after breakfast
You can continue to have clear fluid, clear soup, soft drinks or black tea or coffee (NO MILK)
At 6.00pm the evening before your test
Take both litres of Moviprep following the instructions below
The Morning of your test (up to 2 hours before your test).
You can take essential medicines (as agreed during your clinic/pre-assessment appointment) with a sip of water.
STEP 1
Empty the contents of 1 sachet A and 1 sachet B in to a 1 litre Jug of water.
STEP 2
Stir until the solution is clear
STEP 3
Drink 1 glassful 250ml (¼ litre or
½ pint) of Moviprep every 15 minutes until you have drunk it all.
You can eat any combination of the following:
Adult Moviprep instructions for a morning appointment
Please adhere to the low residue diet advice sheet as certain foods can affect the outcome of your test and may result in a failed test.
How to take Moviprep
- At 6pm empty the contents of ONE sachet A and ONE sachet B in to a jug and add 1 litre (1¾ pints) of cold water and stir until dissolved. (if desired, cordial can be added to taste).
- Drink 250ml (½ pint) of Moviprep mixture every 15-30 minutes until you have drunk it all (usually over about 1-2 hours - no need to rush).
- It is important to drink an additional 500ml (1 pint) of water or fluid of your choice (No Milk).
- Make up your second litre of Moviprep as above and continue to drink, followed by 500ml water or fluid of your choice (No Milk).
- Allow 2 hours after taking the second litre for the Moviprep to work.
- Go to bed when you stop going to the toilet (e.g. 11.00pm or 12.00 Midnight).
Points to Remember
You will experience watery bowel movements so stay close to a toilet.
If you have not had your bowels open after taking the solution please seek medical advice.
If your health has deteriorated since seeing the
doctor or specialist nurse in clinic, please call the consultants who referred you for this test or your GP.
On the day of your test
IT IS IMPORTANT THAT YOU ONLY DRINK CLEAR (NO MILK) FLUIDS UP TO 2 HOURS BEFORE THE TEST.
After your test, you will be advised when to return to your usual diet and medication.
The procedure
When you arrive at your appointment, the Nurse will ensure you are correctly prepared and have followed all of the instructions.
The Nurse will connect a sensor belt around your abdomen and attach a recorder in a bag which is placed over your shoulder.
You will be given a capsule to swallow with a glass of water.
The Nurse will go through the instructions with you about what you will need to do when you get home as you will be required to take some further bowel preparation. These are called ‘Boosters’.
The Boosters will be included in the bag of medicines with the Moviprep® you have been given to take home.
An alarm will sound on the machine throughout the day indicating your next part of the procedure.
Please follow the advice sheet and if you have any concerns or need support, contact the Video Capsule Office on 01785 230508.
Your procedure is complete when the capsule is excreted (passed into the toilet). You will not feel any pain when the capsule passes and the capsule can be safely flushed down the toilet.
Please make sure that you or a relative/friend return the recorder and belt to the Endoscopy Department the following day.
Points to Remember
You will experience watery bowel movements so stay close to a toilet.
If you have not had your bowels open after taking the solution please seek medical advice.
On the day of your test
IT IS IMPORTANT YOU stop drinking 2 hours before the test.
After your test, you will be advised when to return to your usual diet and medication.
Tips:
Some patients report drinking the bowel prep from a sports bottle or with a straw can help take it easier.
If you wish add some orange or lemon squash in with the prep to make it taste better.
Have some normal squash or Lucozade along side the prep to drink.
Don’t rush it—this can make you feel sick.
The results
The images will be downloaded on to the recording device ready to be looked at.
Once a report has been completed, it will be sent back to your referring doctor to act on.
Additional information
The belt will be placed on top of one layer of clothing so please do not wear synthetic materials such as football tops, as this can interfere with the transmission of the pictures.
You can put a jumper or top, if you are able, over the belt if you wish.
If you are happy to, there is no medical reason why you are unable to drive yourself to and from the hospital.
Please make a note of any questions you need to ask using the notes page opposite.
Patency capsule
Introduction
This leaflet provides you with information for the Patency Capsule. It is not meant to replace the discussion between you and your Doctor or
Healthcare Professional but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the Healthcare Team who has been caring for you.
What is a Patency Capsule?
The Patency Capsule is a small pill that is swallowed by the patient at a pre-test before having a Capsule Endoscopy. This indicates whether passage through the bowel is clear for further investigations with the
Video Capsule.
Why do I need to have a Patency Capsule?
The Patency Capsule will identify any blockages in the bowel that may prevent the Video Capsule from safely passing through the bowel.
How does the Patency Capsule work?
The Patency Capsule which you swallow, consists of dissolvable components surrounding a tiny radio frequency identification (RFID) tag that can be detected by X-ray, CT or a Patency Scanner.
How long does the test take?
The Patency Capsule starts to dissolve about 30 hours after it has been swallowed.
You will given an appointment time to return to the Hospital the following day to have a scan to check if you have passed the Patency Capsule.
If the Patency Capsule is not detected, this means that it has been excreted whole and therefore it is safe to continue with the Video Capsule.
It is common for patients to retain the capsule for more than 30 hours, in which case the Patency Capsule will dissolve and pass naturally through your intestine.
Before the procedure
You will be contacted by a Specialist Nurse who will ask you questions about your medical history and will explain the procedure and answer any questions you may have.
How do I prepare for the Patency Capsule?
You will be asked to sign a consent form.
You will need to swallow the Patency Capsule with
a glass of water.
You can eat as normal immediately after you have swallowed the Patency Capsule up until midnight before your appointment.
After midnight, do not eat or drink anything at all.
If you take any medication, take it after swallowing the Patency Capsule.
Are there any risks?
There is only a risk of aspiration (breathing the capsule into your lungs), but this is extremely rare.
What if I pass the Capsule before I return?
If you pass the capsule before returning for your appointment, please call the Capsule Office on the number below and let the Nurses know, as you may not need to attend in person .
If you suffer with any severe abdominal pain, nausea or vomiting that is unusual for you whilst undergoing the procedure, please contact your Nurse or Doctor or go to your nearest A&E if appropriate.
What happens at the appointment?
Using a hand held scanner, the Nurse will check if the Patency Capsule is still inside you.
If the scanner locates it, you will need a CT scan to identify its location.
If it has passed into your large bowel, it will then be safe to proceed with the Video Capsule.
If it has not passed through successfully, it will not be safe to continue.
If you are aged 12-55 and could be pregnant, you will be asked to do a pregnancy test in our department before a CT scan is carried out.
Contact Details
Video Capsule Specialist Nurse
01785 230508
Small bowel endoscopy
What is a Capsule Endoscopy?
This is where a special capsule containing a small camera, is swallowed allowing images of the small bowel to be recorded as it travels through the gut.
The capsule is about the size of a penny.
Why do I need a Capsule Endoscopy?
The small bowel connects your stomach to the large bowel and is difficult to examine properly by conventional methods.
Why do I need to prepare for this procedure?
Your bowel needs to be empty for the procedure so that the Doctor or Specialist Nurse can see the lining of your bowel.
To achieve this you will need to take specific bowel preparations before the procedure, which is explained in this leaflet.
What is bowel prep?
You have been supplied with an oral preparation which is a bowel cleansing agent (also referred to as “bowel prep”). This is called Moviprep®.
If you change your mind at any point, you are entitled to withdraw your consent. You are encouraged to ask questions to help make your decision.
The purpose of this medication is to clear out your bowels and ensure safety and effectiveness of the planned procedure.
You may also require a recent blood test to check your kidney function.
What are the risks of Moviprep® ?
The person prescribing the Moviprep® will have assessed your risk and identified that the medication is appropriate for you
The risks include:
- Developing dehydration.
- Low blood pressure .
- Kidney problems.
Should I still come for the test if my symptoms stop?
It is important that you still come for the appointment, even if your symptoms stop, so that the Doctor can investigate what has been causing your problems and rule out certain conditions.
Taking Moviprep®
The following will apply when taking the bowel preparation:
The Moviprep® will cause diarrhoea and urgency so you will need to stay close to toilet facilities after you have taken it.
If after taking one dose (1A + 1B sachets), of the Moviprep® you have not had your bowels open within 7-8 hours of taking the sachets, please seek medical advice as soon as possible.
- Do not drink dark coloured liquids or milk.
(refer to dietary information).
- If you experience symptoms of dizziness or light headiness (particularly on standing up), thirst or reduction in passing urine, then you may be dehydrated and should seek medical attention.
- All bowel cleansing agents cause diarrhoea so if regular medication is required, it should be taken more than 1 hour or at least 1 hour after taking the Moviprep®.
- Do not take any other medication at the same time as you are taking the bowel prep,
Moviprep® and other medication.
- Please tell the Nursing Staff as soon as possible on the number at the end of the leaflet if you:
- Take any medicines to thin the blood or to prevent blood from clotting (anticoagulants or antiplatelets, such as Warfarin, Rivaroxaban, Dalteparfin or Clopidogrel). If you only take low dose 75mg aspirin, you do not need to call.
- Have diabetes (contact your Nurse Specialist).
- Have an allergy to Moviprep® or its ingredients.
- Please let us know if you are taking any regular medicines at your pre-assessment appointment (including anything you buy yourself over the counter or any herbal or homeopathic medicines).
The diarrhea caused by the bowel preparation can make the oral contraceptive pill less effective. You should continue to take your contraceptive pill as normal but extra precautions (such as condoms) must be used for 7 days after completing the bowel prep.
Refer to the manufacturer’s instructions when taking the Moviprep® for a list of ingredients and allergies. There may be medicines which you are asked to stop taking and these include:
- Heart/Blood pressure tablets e.g. Lisinopril, Ramipril, Perindopril, Captopril, Losartan, Candesartan, Irbesartan, Valsaratan;
- Diuretics (Water tablets) e.g. Furosemide, Bendroflumthiazide, Spironolactone, Amiloride, Co-Amilfruse, Bumtanide, Metolazone, Indapamide, Eplerenone;
- Anti-inflammatory drugs, such as Ibuprofen, Naproxen.
- Tolvaptan: Used for progressive Autosomal Dominant Polycystic Kidney disease or conditions causing low sodium.
Your medication will have been discussed and advice given during your clinic or pre-assessment appointment.
Adult instructions
7 Days before the Test
Stop taking Iron tablets.
3 to 5 Days before the test
You should eat a low residue (low fibre) diet. This reduces the
stool residue in the bowel.
3 Days before the test
Stop taking medications such as codeine and loperamide and stool
bulking agents such as fybogel, as these can reduce the effectiveness of the preparation.
If you suffer from constipation speak to your pharmacist or take
your usual laxatives before you need to start drinking the Moviprep® (do not exceed your maximum dose).
The day before the test
NO solid food after 10.00 am
You can continue to have fluid, clear soup, soft drinks or black tea
or coffee (NO MILK)
At 6.00pm the evening before your test
Take 1 litre of Moviprep®
How to take Moviprep®
1. Between 12.00 noon and 2pm the day before your test, prepare your Moviprep® in advance by emptying the contents of ONE sachet A and ONE sachet B in to a jug and add 1 litre (1¾ pints) of cold water and stir until dissolved. (if desired, cordial can be added to taste).
2. Once mixed, the solution should be kept covered and stored in the fridge until needed. It is easier to take if the mixture is chilled.
3. At 6pm the evening before your procedure, drink 250ml (½ pint) of Moviprep mixture every 15-30 minutes until you have drunk it all (usually over about 1-2 hours - no need to rush). It is then important to
drink, at least, an additional 500ml 1 pint) of water or fluid of your choice. (No Milk).
4. You are advised to continue to drink plenty of clear liquids up until Midnight. Any essential medications can be taken with a small glass of water up until 2 hours before your appointment.
You will experience watery bowel movements so stay close to a toilet. If you have not had your bowels open after taking the solution please seek medical advice
STEP 1
Empty the contents of 1 sachet A and 1 sachet
B in to a 1 litre Jug of water.
STEP 2
Stir until the solution is clear
STEP 3
Drink 1 glassful 250ml (¼ litre or ½ pint) of Moviprep
every 15 minutes until you have drunk it all. There is no need to rush.
The procedure
When you arrive at your appointment, the Nurse will ensure you are correctly prepared and have followed all of the instructions and you will be asked to sign and complete a Consent Form.
- The Nurse will connect a sensor belt around your abdomen and attach a recorder in a bag which is placed over your shoulder.
- You will be given a capsule to swallow with a glass of water.
- The Nurse will check that the capsule has passed into your stomach by looking at a real time view screen on the data recorder.
- You will be then asked to go for a walk for 30 minutes.
- When you return, the Nurse will check the progress of the capsule and if the capsule has entered the small bowel successfully, you will be free to return home.
- You will be shown how to remove the equipment before you return home so that you can remove it before you go to bed.
What happens when I return home?
You can have clear fluids 2 hours after you swallowed the capsule.
You will be able to eat a light lunch 4 hours after swallowing the capsule unless the Nurse tells you otherwise.
The capsule will move naturally through your digestive system whilst you continue with your normal activities.
Remember do not sleep wearing the equipment as this can slow down the capsule transit.
If you notice the capsule pass before you go to bed, you can remove the equipment as the procedure is complete.
Please make sure that you or a relative/friend return the recorder and belt to the Endoscopy Department the following day.
What are the risks?
A small bowel capsule endoscopy does have its risks but major and serious complications are rare.
These risks will be discussed with you before you sign the consent form. These include:
- The capsule may be inhaled into the lungs.
- The capsule might get stuck in your small bowel. If
this occurs, then it may be necessary to remove the capsule.
- The capsule may need to be repeated with extra bowel preparation if the images taken are of poor quality and we are not able to see the small bowel clearly.
- The capsule may remain in your stomach for too long and not all of the small bowel lining may be visible before the battery runs out. To help reduce this risk, the Nurse will check the capsule has left your stomach and entered the small bowel before you leave the department.
The results
The images will be downloaded on to the recording device ready to be looked at.
Once a report has been completed, it will be sent back to your referring Doctor to act on. This can take up to 4-6 weeks.
Additional information
The belt will be placed on top of one layer of clothing so please do not wear synthetic materials such as football tops, as this can interfere with the transmission of the pictures.
You can put a jumper or top, if you are able, over the belt if you wish.
If you are happy to, there is no medical reason why you are unable to drive yourself to and from the hospital.
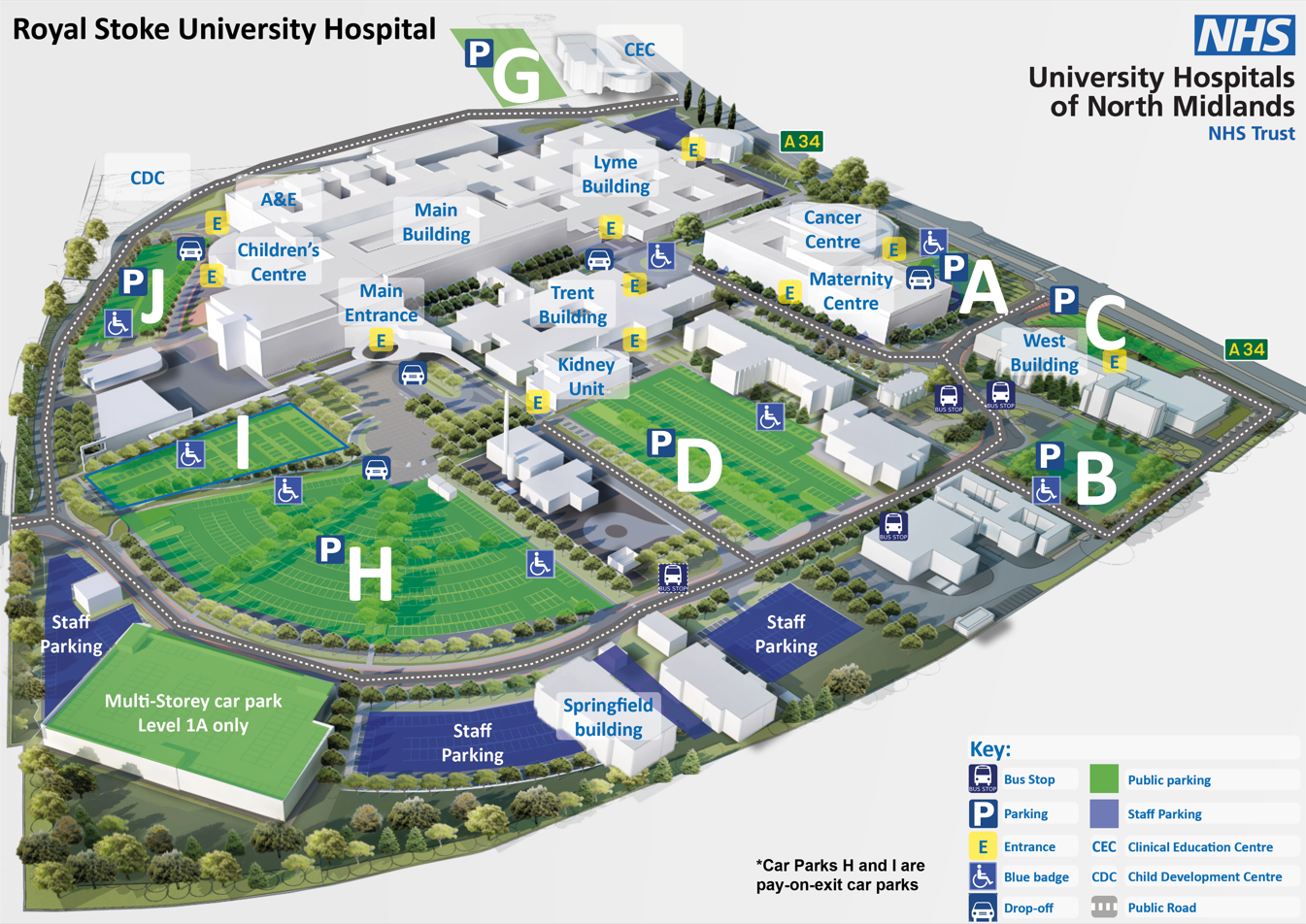
 Please note, car parking charges apply. There is a shuttle bus service running between Royal Stoke and County Hospital. Please call 01782 824232 to arrange a place on the bus.
Please note, car parking charges apply. There is a shuttle bus service running between Royal Stoke and County Hospital. Please call 01782 824232 to arrange a place on the bus.



 University Hospital North Midlands (UHNM) Endoscopy Unit is a Joint Advisory Group (JAG) accredited training centre which sits within UHNM as a teaching hospital. The JAG encompasses national best practice standards for endoscopy. Hospitals have to go through a rigorous assessment process to become an accredited Trust, and are then subject to annual compliance reviews. Only those hospitals that are awarded this accolade are able to apply to become a training centre. More information on JAG can be found here
University Hospital North Midlands (UHNM) Endoscopy Unit is a Joint Advisory Group (JAG) accredited training centre which sits within UHNM as a teaching hospital. The JAG encompasses national best practice standards for endoscopy. Hospitals have to go through a rigorous assessment process to become an accredited Trust, and are then subject to annual compliance reviews. Only those hospitals that are awarded this accolade are able to apply to become a training centre. More information on JAG can be found here