Surgery for lung cancer
The type of surgery you might have depends on where in the lung your cancer is, how big it is, and your general health.
After your appointment in Lung Cancer clinic (either face to face or on the telephone) you will have been advised that you will require Thoracic surgery. This decision would have been made from the Lung MDT meeting which is made up of a team of highly specialised professionals who have looked at your case specificity and feel that surgery would be beneficial. If you are happy to go ahead, you will be referred to the surgical team. This will be to discuss surgery options and review your current fitness for surgery.
The type of surgery you might have depends on where in the lung your cancer is, how big it is, and your general health.
You should have been given or sent in the post the Roy Castle booklet ‘My surgery’. This booklet is very informative pre and post surgery. If you have no received a booklet please contact your Lung CNS advising you would like one.
to look at the online version please see the link below
www.roycastle.org/app/uploads/2020/02/My-Lung-Surgery-Feb-2020-Online.pdf
We fully understand this will be a worrying and anxious time for you. Hopefully the information below will help support by giving you some helpful information. If you have any further questions please Contact the Lung CNS team.
Types of surgery for lung cancer:
These are the different methods of surgery used. The method will be decided by your surgeon and may vary due to the location and size of the nodule.
- Thoracotomy / Open surgery- An incision is made around the side of your body, below your shoulder blade and between your ribs. The ribs are spread to get access to the lungs.
- Video Assisted Thoracoscopic Surgery (VATS) / Keyhole Surgery- Your surgeon uses video camera and one to three small cuts (1-5cm) to perform the operation. Incisions are generally made under the arm and/or just below the shoulder blade. The ribs are not spread.
- Median Sternotomy- This is a cut made vertically down the chest over the breastbone, which allows the surgeon to see both the left and right side of the chest. It is occasionally used for some lung operations.
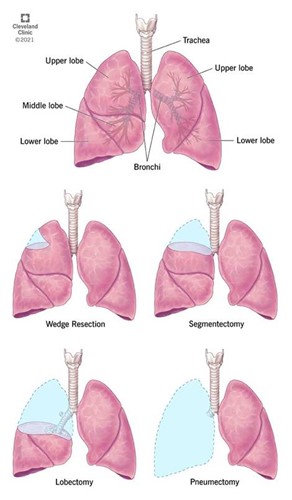
- During surgery, a part or all of a lung may need to be removed, particularly if it contains a tumour. The amount of lung that is removed will depend on location, size of your tumour, biopsy results, spread of your cancer, and sometimes on your fitness levels.
There are different types of surgery and these are done by specialist lung surgeons
- Segmentectomy/Wedge resection: Each lobe of the lung is made up of several segments. If your fitness will not allow more extensive surgery, or the cancer is small, your surgeon may be able to remove just a segment, or a small piece of lung tissue surrounding the cancer, rather than the whole lobe.
- Lobectomy: This is the most common operation for lung cancer. It is chosen if your cancer is contained in a single lobe, and you are reasonably fit. There are 2 lobes on the left and 3 on the right. It involves the removal of a lobe of the lung. The remaining lung will expand to fill the space left by the tissue that has been removed.
- Bi-lobectomy: This is the removal of two lobes of the lung on the right side.
- Sleeve lobectomy: This is removing part of the main airway or lung artery, with the lobe being removed. The two ends are sewn together. This procedure can avoid removing the whole lung for some patients.
- Pneumonectomy: This means removing a whole lung and is chosen when the tumour extends beyond just one lobe. You may feel breathlessness after surgery; that is more common after this procedure. Along with removing the tumour, using one of these techniques, the surgeon will remove lymph glands or nodes from your chest. This helps decide if further treatment, such as chemotherapy, is needed.
Before your operation for lung cancer:
- At your first appointment you will meet the surgeon and they will be able to discuss any questions or concerns about the surgery and post-operative (after surgery) care. They may also send you for further investigations if required. They will then list you for surgery. You will be updated with the surgery date either by the surgeons or by the surgical secretaries
- Before admission you will need to attend pre-assessment (sometimes called ‘Pre-Ams’). This is usually not on the same day as you surgical appointment. This can take up to 45mins. The assessment will include the nurse taking your medical history as well as routine test such bloods, MSSA/MRSA swabs, your height and weight, and ECG (heart tracing)
- Please see the link below for further information and questions you may have about this appointment.
- https://www.uhnm.nhs.uk/our-services/pre-admission-management-service-preams
Preparing for surgery:
There are different ways you can prepare in the weeks before your surgery . This includes:
- Keeping active
- Stopping smoking
- Eating well
- Stocking up on extra foods
If you live alone it is a good idea to have support from a neighbour or friend.
Please see the links below for more information from Macmillan and a short video from Roy Castle
https://www.macmillan.org.uk/cancer-information-and-support/treatment/types-of-treatment/surgery
https://www.youtube.com/watch?v=uUqFx8RFhl0
What I need bring into hospital:
- Comfortable and practical clothes
- Own PJ’s and nightdresses- The ward do have a supply of PJs and nightdresses, but patients are encouraged to wear their own clothes as soon as practical
- Pair of slippers or shoes that can be worn at all times on the ward
- Toiletry bag –Soap/ Shower Gel. Toothpaste, toothbrush, comb, razor, shaving foam and deodorant. The ward will supply towels, flannels and soap
- Books, Mobile phones and Tablets are all allowed on the war. There is a free UHNM Wifi service which can also be used
- Your regular medications or inhalers that you take.
Admission to hospital:
- During you inpatient stays Pre and Post surgery, you will be on ward 223. Which is a ward based for patient having cardiothoracic surgery
- Ward 223 is located in the main building on level 1. The telephone number for the ward is 01782 676223/675223.
- Some patients require closer monitoring after surgery so they would require a short period of time in Critical care Pods 1&2. This is located in the main building on lower ground 2. You will be transferred back to ward 223 as soon as possible and once the doctors are happy with your condition.
- Once they are happy you are stable to go home they will discharge you from ward 223
- Please see the link for location and Numbers for ward 223 and visiting times
- Ward 223 | University Hospitals of North Midlands NHS Trust (uhnm.nhs.uk)
- Everyone's length of stay will vary from 2-10 days but the average time is 3-5 days
- Before you come into hospital you will need to think about how you are going to get home once discharged as you will not be able to drive for at least 6 weeks following the operation.
- 72 hours prior to your admission date you will be required to have Covid-19 test. Some patients may just required Lateral flow test but you will be updated on which one is appropriate for you by the surgical sectaries. Their number is 01782 675962
Admission/Day of surgery:
The day before your surgery you need to ring the ward at 4pm on 01782 676223 to see if there is a bed available for you that night.
Due to busy nature of this ward, and where you are on the theatre list, there may not be a bed available that night. If so, you will need to arrive at on the ward at 08:30 the following morning.
You may have a short wait for the bed so you may want to bring something to keep you occupied.
You will need to have a shower the night before with the Hibiscrub which you will have been given at the pre assessment appointment .
This can be done on the ward, if you are admitted the night before surgery, or if you are at home.
When you are admitted to the ward, nursing staff will ask you to take a bath or shower and put on a clean hospital gown. They will also provide you with compression stockings to help prevent blood clots developing during and after surgery. Your surgeon will use a special marker pen to mark the area on your skin where they plan to do the operation.
- You will not be allowed anything to eat or drink from midnight unless instructed otherwise. You can have a small slip of water with your medications but you will need to check with Nurse In charge which medications you are able to take,
- If you have been given glucose drinks at the pre assessment clinic, you need to take one at 10pm the night before surgery, and the other drink at 6am the next morning.
- If you require any medication to make you feel relaxed or comfortable prior to surgery, you can discuss this with the staff on the ward once you are admitted.
- Once they are ready for you to go to surgery the surgical theatre staff will send a porter to take you down to theatre. In the anaesthetic room the staff will check your wristband and consent form. You will have a general anaesthetic so you can't feel anything during the operation: this sends you into a deep sleep.
- Once you are asleep, a breathing machine (ventilator) will support your lungs. The ventilator is connected to a tube inserted down your windpipe
After lung cancer surgery:
After your operation you will be transferred to the recovery unit and may stay there for a few hours. When they think you are stable they you will be transferred back to the ward.
You may feel tired and a bit groggy but this is normal post surgery due to the anaesthetic.
You will be able to have visitors post surgery.
You will also have some medical equipment attached after surgery which may include:
- Up to three chest drains to remove fluid and air from your chest and help your lungs to re-inflate.
- One or two drips in your hand(s) so we can give you fluids and / or medicines.
- Neckline (a drip that goes into a vein in your neck) to monitor your blood pressure and fluid levels.
- Bladder catheter (a tube going into your bladder) to drain away urine.
- Oxygen mask (over your mouth and nose) or nasal prongs (two soft plastic tubes under nostrils) to provide oxygen after your surgery if needed
Most patients need chest drains after surgery. Chest drains are designed to remove the blood, fluid and air that collect within the chest cavity after surgery. The drain is a one-way system that prevents fluid and air from returning to the chest. One end of a plastic tube is placed in your chest and the other end goes into a drainage bottle. The tube is held in place with a stitch. The end of the tube is placed between the rib-cage and the lung and leads out to a drainage bottle.
You can walk around with a chest drain, but remember to carry the drainage bottle with you.
Always carry the bottle below the level of your waist. If you lift it above your waist, fluid from the bottle might flow back into the space between tour lung and rib-cage.
If the drainage is on a wall suction unit, you will need to stay close to your bed.
While in bed, keep the drainage bottle on the floor.
Avoid trapping, kicking or folding the tubes as this may stop them from draining.
Try to avoid the tubes getting caught in clothing or equipment to prevent pulling on them as this may cause discomfort and pain
Do not leave the ward.
Once the surgeons is happy the drain can be removed this will be done by the nursing team.
The Nurse might ask you to breathe in a particular way while the drain is removed. It is pulled out gently.
This procedure can feel a little uncomfortable, but only lasts a few seconds. If you have any discomfort after we have removed the drain, you can take painkillers.
Some patient may need to go home with a chest drain. The nursing team will provide you with an information leaflet on how to manage the drain and you will be able to contact the ward directly if you have any questions or concerns. The surgeons will review the drain as an outpatient and decide when it needs to be removed.
http://sales.rocketmedical.com/media/attachment/file/r/o/rocket_ambulatory_bag_user_guide.pdf
Pain Relief:
You are likely to be uncomfortable after the surgery and it is not always possible to take all the discomfort away. However, it should be controlled. There are several ways this can be managed:
- PCA (Patient controlled Analgesia) you will be able to control your own pain by pressing a button that will give you a set measured amount of pain killers from a syringe which will be given by a vein in your arm. This will be for the first 24-48hours after surgery
- A paravertebral catheter may be used instead of an epidural for pain relief. This is a small tube placed into the space between the back bones (vertebrae) near the thoracic spinal nerve.
- Once you are eating and drinking again, they will give you pain relief tablets at regular intervals to keep you as comfortable as possible. You will be prescribed tablets and will be given these to take home. If you feel your pain relief is not adequate you can speak to the nurses and doctors on the ward prior to discharge.
Mobilising after Surgery:
- You’ll be encouraged to mobilise as soon as possible after the operation. You will see a physiotherapist or specialist nurse who will encourage you to cough, deep breathe, move around and exercise your arms and shoulders. This is particularly important on the operation side of your body to prevent stiffness or a frozen shoulder.
- Once you are steady on your feet you can walk around on your own, as long as you feel comfortable. This encourages your lungs to expand and may let you get home faster. Keeping active after lung surgery will improve your recovery. It will have a positive effect on your heart, muscles and lung capacity.
- Please see the Roy castle surgical booklet for more information on this
- https://www.roycastle.org/app/uploads/2020/02/My-Lung-Surgery-Feb-2020-Online.pdf
Discharge from hospital:
- You'll probably be able to go home 3 to 10 days after your operation. However, it can take many weeks to recover fully from a lung operation.
- Before you go home the nurse will check your wound, make sure there are no concerns. Most of your sutures are dissolvable. However, the sutures from the chest drain are not and these will need to be removed 7-10 days after the drain is removed.
- The ward will arrange for your GP practice or district nurse to remove your sutures
- If you have any problems with your wound when you are at home, such as redness, soreness, or if the wound feels hot to touch or oozes liquid, please see your GP or call the ward for advice
- Before you are discharged home from the ward you will be give:
- 28 day supply of medications- This may include Dalteparin injections (to prevent blood clots)
- A doctors letter for your GP and yourself
- Support stockings which need to be worn the first few weeks after your surgery to prevent blood clots. You will need someone to help you with these as they take a considerable amount of effort to put on. You will have two pairs and these can be washed in the washing machine.
Recovering at home:
- After your operation, you may feel stressed, anxious or depressed. Being affected emotionally is normal. It may help to talk about how you feel with a member of your family, a friend or your nurse specialist. Sometimes your friends and family need to talk things over as well.
- When you go home, you'll need to exercise gently to build up your strength and fitness. This can be done my completing daily exercises and eating well post-surgery as it can be normal to have a reduced appetite.
Please see Roy castle for recovery at home
https://www.roycastle.org/app/uploads/2020/02/My-Lung-Surgery-Feb-2020-Online.pdf
Problems after lung cancer surgery:
- There is a risk of problems or complications after any operation. Many problems are minor but some can be life threatening. Treating them as soon as possible is important.