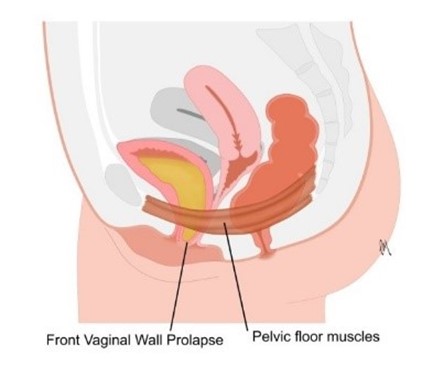
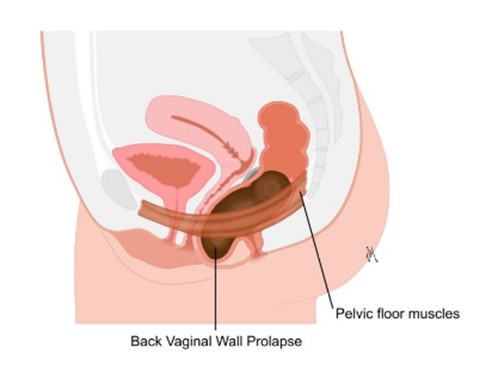
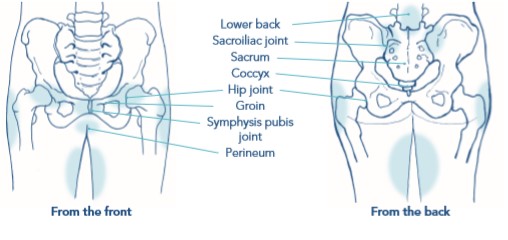
Sometimes a doctor or a midwife may have needed to make a cut in the area between the vagina and anus (perineum) during childbirth. This is called an episiotomy.
An episiotomy makes the opening of the vagina a bit wider, allowing the baby to be born more easily. Sometimes a woman’s perineum may tear naturally as their baby comes out.
Up to 9 in 10 first time mothers who have had a vaginal birth, will have some sort of tear, graze or episiotomy. Stiches should heal within 1 month of the birth.
Coping with Pain
It is common to feel some pain after an episiotomy or perineal tear.
Painkillers such as paracetamol; can help relieve pain and is safe to use if you are breastfeeding.
It is also considered safe to take Ibuprofen while you are breastfeeding, but check with your doctor, midwife or obstetrician first. Aspirin is NOT recommended.
It may be necessary to treat severe pain with stronger prescription only painkillers such as codeine. This may affect your ability to breastfeed safely. Your GP or midwife can advise and support you with this.
Good hand washing and hygiene is important. Clean your wound with water. Unperfumed soaps can be used for general washing in that area & change your sanitary towels regularly.
Exposing the stiches to fresh air can help the healing process. Taking off your underwear and lying on a towel on your bed for around 10 minutes once or twice a day may help.
It's unusual for pain after an episiotomy to last longer than 2 to 3 weeks. If the pain lasts longer than this, speak to a doctor, midwife or health visitor, and ask to be referred to the Pelvic Health Clinic for a follow up appointment. You can also use the self- referral link on the homepage to access the service.
Useful links:
POGP booklet – Perineal healing after a vaginal birth
POGP booklet - Fit for the future
POGP booklet - Exercise and advice after pregnancy
RCOG-Perineal tears and episiotomies in childbirth
NHS episiotomy and perineal tears
(Please note UHNM does not take responsibility of accessibility of external websites and documents)