This leaflet has been written to help you understand your diagnosis. If you have any questions or concerns, please do not hesitate to contact your specialist nurse.
What is advanced prostate cancer?
This is a term used to describe a prostate cancer that has spread outside of the prostate gland to nearby organs and structures and may also have spread to distant sites such as the bones (metastases). This leaflet has been written to help you understand more about the treatment options available to you.
What symptoms might I expect?
The symptoms experienced by men with advanced prostate cancer are usually linked to the effect on the prostate gland or the area of spread.
These symptoms might include:
- Waterworks problems
- Blood in the urine (haematuria)
- Pain in the bones
Some men may not experience any of these symptoms.
How will my prostate cancer be treated?
The aim of your treatment will be to control the cancer rather than cure it. Hormone Manipulation Therapy will be the key treatment. Prostate cancer needs testosterone to grow and Hormone Manipulation Therapy stops the
production of this hormone. By stopping testosterone from reaching your tumour, your cancer can be treated effectively. This treatment is effective for varying lengths of time and differs with individuals.
How is hormone manipulation treatment given?
These are the treatment options open to you; Hormone injections, which reduce the testosterone level in your body. Surgical removal of the part of the testicles, which produces testosterone called a bilateral orchidectomy. Both options are equally effective. You should read this leaflet alongside the leaflet entitled ‘Patient information for bilateral orchidectomy for prostate cancer’ before you make your decision.
Are there any alternatives to having hormone therapy and what would happen if I decided not to have this treatment?
Your consultant will have explained the different treatment options available to you and what would happen if you decided not to have any treatment at all. The choice about which treatment is best for you will be made together with your doctor or nurse. This will be based on the risks and benefits of the treatments and your individual circumstances. Without treatment your cancer may progress and it may be difficult to control any symptoms you have.
Are there any risks or long term effects involved in having hormone therapy?
Yes, there are side effects to nearly all treatments. Therefore you must consider the following side effects before deciding to undergo this treatment.
- Hot flushes and night sweats – these are common and may be severe in the first six to 12 months.
- You may also notice that you have to shave less often.
- Tiredness
- Weight gain
- A reduced sex drive
- Impotence – you will probably experience impotence once you start treatment. This is the inability to achieve an erection.
- Thinning of the bones - osteoporosis
- Breast swelling and tenderness
Less common side effects are:
- Joint pain
- Changes in blood pressure
- Skin rashes
- Low mood
There may be some treatment that can be given to you if any of these side effects are particularly troublesome. Speak to your GP, consultant or specialist nurse if you suffer from any of them.
How will my prostate cancer be monitored?
Hormone therapy works for a varying period of time and your PSA level informs the doctor or nurse of its effectiveness. It is anticipated that the treatment will become less effective in time which will require additional treatments. Your PSA level and symptoms will determine at what point new treatments will be introduced.
When am I likely to receive what treatment?
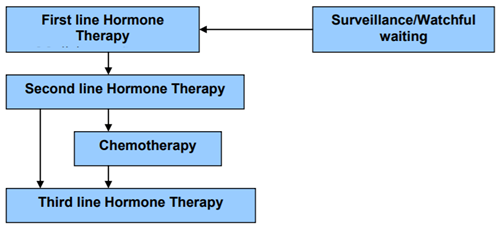
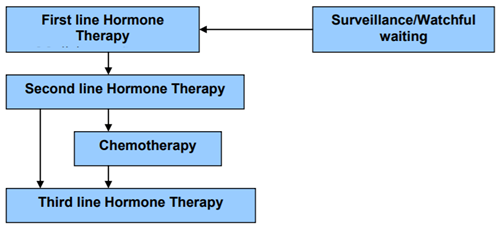
Hormone therapy is most often started when your diagnosis is made. This is called ‘first line hormone therapy’ meaning the first hormone treatment for you. There are several treatment options which can follow this first line therapy and as each treatment becomes less effective a new treatment option will be considered.
Diagnosis and treatment pathways
What further symptoms might I experience?
Pain is a symptom that worries people most with cancer. Prostate cancer which has spread into the bones can cause pain. This can be successfully
controlled with either the correct pain killers or with a dose of radiotherapy (X-ray treatment to the affected bone). Other symptoms you might experience include bleeding or increased difficulty in passing urine and osteoporosis (thinning of the bones). Please inform your GP, consultant or specialist nurse if you suffer any of these symptoms.
One rare complication of advanced prostate cancer is from the cancer affecting the bones in your spine. This can damage the nerves which can cause symptoms of numbness or tingling to your feet. This is called ‘spinal cord compression’ and requires urgent attention and treatment. If you experience this symptom please contact you GP immediately. Management of potential symptoms can be introduced when ever necessary throughout your treatment.
Pain > Analgesics
Bone complications > Local radiotherapy
Water work problems > Medicines or surgery
Bone Thinning > Bisphosphonate medication
Spine complications > Steroids and/or Radiotherapy
Am I suitable for a trial?
There may be an opportunity to participate in a clinical trial. If a suitable trial is available to you this would usually be discussed with you, however please ask your consultant or nurse specialist if you would wish to be considered.
Where can I get further information and support?
Many people living with cancer may worry about what the future holds. Concerns about tests and treatments are common. Some people find the
information given to them following a complicated clinic visit daunting and difficult to remember. Karen Smith is a Clinical Nurse Specialist in Urology who is available for you to call with any worries, questions or problems. Please telephone Karen on 01782 553820. (Answer machine available)
It may be helpful if you make a list of your concerns to help you remember to ask your consultant or specialist nurse the questions that are important to you.
Who else will be involved and able to help me?
Various people may become involved in your care. District nurses who work closely with your GP may visit you at home. Palliative care nurses
often become involved in patients care that have cancer. Palliative care nurses specialise in helping people with symptoms caused by their cancer. It is recommended these nurses get to know you early in your treatment and not when symptoms have become unbearable. Your consultant, specialist nurse or GP can ask the palliative care nurses to meet with you.
Useful Contacts
Karen Moore, Clinical Nurse Specialist
Urological Cancer. Tel; 01782 553820
(Answer machine available)
There is also a North Staffordshire Prostate Cancer Support Group, which is open to anyone affected by prostate cancer. If you wish to speak to someone receiving the same treatment this can be arranged for you either through the support group or your Nurse Specialist.
The North Staffs Prostate Cancer Support Group Held on the 3rd Wednesday of every month 6pm till 8pm
Joiners Square Community Centre
Corns Street
Hanley
Macmillan Cancer Support and Information Centre
University Hospital of North Midlands
Open for drop in sessions:
Monday – Thursday 10am until 12.30pm and 2pm until 4pm
Tel: 01782 554363. (Answer phone available out of hours)
National sources of further information
Macmillan cancer line 08088082020
Website: www.Macmillan.org.uk
BACUP (cancer information service)
Free phone 0800181199
Website: www.cancerbacup.org.uk
Cancer Help UK
Website: www.cancerhelp.org.uk
The Prostate Cancer Charity
Tel. 0845 300 8383
Email: info@prostate-cancer.org.uk
Website: www.prostate-cancer.org.uk
Prostate Cancer Support Association
Tel. 0845 6010766
Institute of Cancer Research
Tel. 020 7352 8133
Website: www.icr.ac.uk
Cancer Backup Information Service
Freephone 0808 800 1234
The Sexual Dysfunction Association
Tel. 0870 7743571
Website: www.impotence.org.uk
Cancer Help UK
Freephone 0800 226 237
Website: www.cancerhelp.org.uk